Does a tight scalp cause pattern hair loss? This question recently resurfaced in hair loss forums… sparking heated debate from scalp tension supporters and opposers.
The supporters: scalp tension must contribute to hair loss. Why? Because balding men and women tend to have chronically tight scalps. This tension tends to match the pattern and progression of hair loss. And when we look at the effects of chronic tension in other tissues, we see near-perfect overlap with the biomarkers of a balding scalp: increased androgen activity, excess collagen deposition, tissue degradation, and hair loss.
Thus, scalp tension must be involved in pattern hair loss. Scalp tightness not only fits within the current androgenic theory, but also helps to answer many questions that the androgenic theory can’t – like why dihydrotestosterone (or DHT) increases in balding scalps… why DHT leads to hair loss in the scalp but hair growth in the chest and face… and why androgenic alopecia occurs in a specific pattern and progression.
But there’s one thing scalp tension advocates can’t explain: hair transplantation results. In fact, hair transplantation studies are the strongest opposition against the scalp tension theory. They’re also the rallying cry for the theory’s opposition.
The opposers: the entire idea that scalp tension contributes to pattern hair loss hangs on one major assumption: that our scalp environment influences our hair follicles’ ability to grow hair. However, this assumption is false. It was disproven in 1959 with the first study on hair transplantations. This study showed that…
- Non-balding hairs transplanted to balding regions will keep growing normally.
- Thinning hairs transplanted to non-thinning regions will keep balding at the same rate as other balding hairs in the scalp.
These findings, according to critics, demonstrate that androgenic alopecia has nothing to do with our scalp environment (or scalp tightness). Rather, pattern baldness must be genetically programmed within the follicles themselves. In other words, it’s the interaction between androgens and genetics that likely determines our hair follicles’ predisposition for hair loss and our baldness “clock”… not scalp tension.
So who is right? Who is wrong? And do these hair transplantation studies overturn the scalp tension-hair loss hypothesis… or are we missing something in our logic?
That’s what this article is for.
This is part two of a three-part series on scalp tightness and androgenic alopecia.
In the first article, we explored the science behind how scalp tension might contribute to androgenic alopecia. Now it’s time to build the scalp tightness counterargument.
First, we’ll dive into the scalp tension theory’s opposition and uncover the hair transplantation studies that changed the trajectory of hair loss research. Then we’ll reevaluate those studies in light of new evidence… and see if the conclusions from 1959 still hold today.
Finally, we’ll present new evidence to suggest that our scalp’s environment might influence our hair follicle’s ability to grow. In doing so, we’ll revisit the concept of donor dominance… and list some discrepancies in its theory.
By the end, we should have a firm understanding of the arguments for and against the scalp tension theory of androgenic alopecia. That way, you can decide what to believe. After all, hair loss research is always up for reinterpretation.
If you have any questions, I’m happy to address them in the comments.
The argument against the scalp tension theory: hair transplantation studies
In 1950, the scalp tension theory of androgenic alopecia had picked up steam in scholarly journals. But it wasn’t until 1959 that researchers figured out how to test its plausibility.
That year, a researcher named Dr. Orentreich set up an experiment to understand which factors influence why we go bald. His major question: is baldness due to a hair follicle’s environment (i.e., its surrounding tissue)… or is it due to the hair follicle itself?
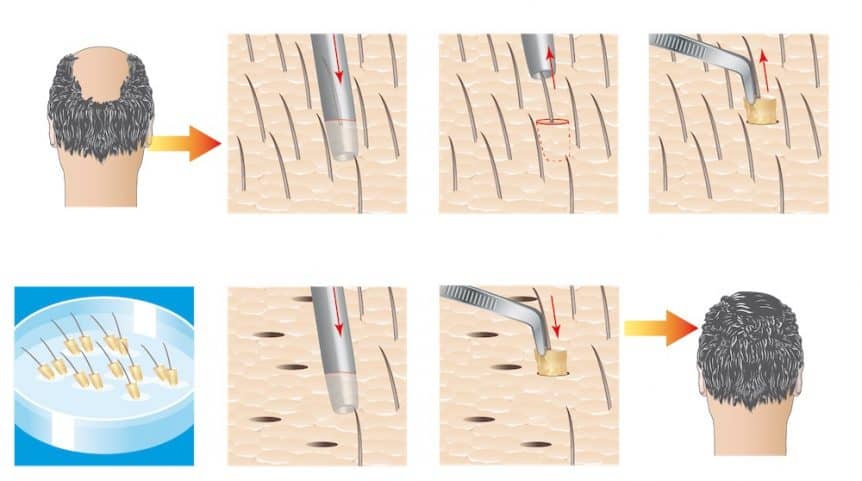
Dr. Orentreich thought of an ingenious way to test this. Hair transplantations. Specifically, he wanted to see if a balding hair transplanted out of a balding scalp would continue to bald… and if a healthy hair transplanted into a balding scalp would continue balding. He figured that if balding had anything to do with our scalp environment, healthy hairs moved to balding regions would start to bald – and balding hairs moved to healthy regions would stop balding.
So he gathered patients with androgenic alopecia (AGA) and performed his tests:
- He took skin grafts (6-12mm punch biopsies) of balding scalp regions and transplanted those grafts into non-balding parts of the scalp.
- He took 6-12mm punch biopsies of non-thinning scalp regions and transplanted those biopsies in balding parts of the scalp.
So, he got busy observing (and waiting). Years later, he published his findings. What were the results?
Balding hairs keep balding, and non-balding hairs keep growing… no matter where we put them
That’s right. After 2.5 years of observation, Oreintreich found that…
- Non-balding hairs transplanted to balding regions will keep growing normally.
- Balding hairs transplanted to non-thinning regions will keep thinning at the same rate as balding hair at the top of the scalp.
Thus, he concluded that our scalp environment had no influence over a hair follicle’s determination to start thinning. To quote directly from his study…
“…The determinants of growth of strong scalp hair or of baldness lie within the local skin tissues of a full-thickness graft and suggest that the pathogenesis of common male baldness is inherent in each individual hair follicle. Probably each individual follicle is genetically predisposed to respond or not to respond to androgenic and/or other influences that inhibit its growth”
Dr. Orentreich referred to scalp hair follicles as donor dominant – meaning that scalp hairs retain all of their characteristics regardless of where they’re placed. In his words…
“…The transposed grafted skin maintains its integrity and characteristics independent of the recipient site.”
These findings undermined the scalp tension hypothesis entirely. But this was just one study. In order to be sure, we’d need to see these results occur again… and again.
Over the next two decades, that’s exactly what happened.
Follow-up studies confirm Dr. Orentreich’s hair transplantation findings
In 1979, a researcher took composite skin grafts of balding, non-balding, and bald scalp regions from a 29-year old patient, then transplanted those skin grafts to the forearm and observed their hair growth over the next several months.
His findings? When those scalp skin grafts were moved to the forearm, bald hairs stayed bald, thinning hairs continued to thin, and non-thinning hairs remained thick and healthy.
Then in 1982, doctors from the Oregon Regional Primate Center used a similar skin graft procedure to transplant the hairs of balding primates from the backs of their scalp (i.e., where hair was healthy) to the front of the scalp (i.e. where these stump-tailed macaques were experiencing human-like pattern hair loss).
Eight years later, the primates’ donor hairs were still alive – despite the fact that their surrounding follicles had succumbed to baldness. Again – the evidence confirms that transplanted hairs don’t miniaturize – and that hair follicles aren’t affected by their environment.
So… is the scalp tension theory officially debunked?
Well, let’s review the evidence:
- Early hair transplantation studies show that transplanted hairs don’t miniaturize… even when they’re transplanted into “tense” (i.e., balding) scalps
- Some of those studies show that balding hairs keep miniaturizing… even when they’re removed from a balding environment and placed on the forearm.
Based on these findings, it’s completely rational to assume that the scalp tension theory is invalid. In other words, our scalp environment does not influence a hair follicle’s growth. Hair transplantation studies confirm this belief. And as such, the scalp tightness theory is debunked. Right?
Well, not so fast.
We’ve really only built a straw-man’s argument against the scalp tightness-pattern hair loss hypothesis. Why? Because we’ve yet to address the two elephants in the room.
Elephant #1: relieving scalp tension improves AGA outcomes
There’s evidence that relieving scalp tension – either through mechanical offloading or Botox injections into “tight” scalp muscles – improves hair counts in AGA sufferers… and on-par with the effectiveness of finasteride. We discussed these findings in our original scalp tension article.
So if scalp tension doesn’t contribute to AGA… for some reason, relieving scalp tension helps reverse it. Go figure.
Elephant #2: hair transplant studies don’t answer every question needed to refute the scalp tension-AGA hypothesis
Let’s look at these studies’ conclusions again. What are they saying?
If we take a chunk of skin from the back of our heads and insert it into a balding region, that skin’s hair will continue to grow for several years.
But if we’re to refute the scalp tension hypothesis, that’s not what we should be testing.
This is because we haven’t yet isolated the variable to which we’re making inferences… the actual hair follicle.
Rather, these studies evaluate how entire landscapes of skin behave when moved to different locations of the body. Accordingly, here’s how the conclusions of those studies should’ve read:
When harvesting 6-12mm skin punch biopsies, the 20-80 hair follicles within those biopsies retain their growth characteristics regardless of where they are transplanted on the scalp, even in men with AGA.
Now, what does this conclusion not tell us?
- If a hair follicle’s immediate environment (i.e., its skin tissues and surrounding hair follicles) influence its growth characteristics.
- If older hair transplants “strip” techniques achieve the same lasting results as individual hair follicle transplants
- If transplanted skin experiences the same tensile environment as surrounding skin
Again, these hair transplantations are incredibly important. But they don’t answer these questions. And if we’re to refute the scalp tension hypothesis, we need to evaluate each of these questions carefully.
That’s what the rest of this article is going to do. And in doing so, we’ll see issues in using early hair transplant studies as evidence against the scalp tightness theory.
1. Does a scalp hair follicle’s surrounding environment influence its growth characteristics?
Contrary to what those initial hair transplant studies suggest, a hair follicle’s environment does influence its behavior. We’ve seen this demonstrated in three major ways:
- Scalp hairs change growth behaviors depending on where they’re transplanted
- Balding human hair, when transplanted on mice, can regenerate in one hair cycle
- Hair follicles directly next to each other can coordinate / hair growth
Let’s take these one-by-one.
Scalp hairs change growth rates depending on where we transplant them
In 2002, a team of researchers published a study that revised aspects of Orentreich’s “donor dominance”. The team’s first research question: over a three-year period, what happens if we transplant scalp hairs from the back of our heads to our lower leg?
The results: 60% of transplanted hairs survive, and the ones that survive grow at about half the speed of regular scalp hairs.
Their second research question: what happens if we re-harvest those scalp-hairs-turned-leg-hairs and move them back to the scalp (or more specifically, the nape of the neck?)
The results: those re-transplanted hairs – which were once scalp hairs, then leg hairs, and now are neck hairs – grow at a slower speed than non-transplanted scalp hairs. However, they grow at the same speed of hairs transplanted directly from the scalp into the neck.
The takeaways: scalp hair follicles adapt to growth rates set by their surrounding environment. Thus, scalp hair follicles can be influenced by the location in which they are transplanted.
Moreover, a follow-up study showed that chest hairs, when transplanted into balding scalps, grow longer to match the length of surrounding (but still balding) scalp hairs.
Together, these findings suggest that scalp hair follicles are not 100% donor dominant… and that scalp environment can influence the behavior of its recipient hairs.
As for why? The investigators weren’t sure. But they hypothesized this could be due to “recipient site characteristics such as vascularity, dermal thickness or skin tension.”
Again — that’s not to say that donor dominance is invalid — or that scalp hairs transplanted into balding regions won’t grow. We’re just highlighting that recipient sites of scalp hairs can influence that hair’s growth characteristics — which goes against the idea that scalp hairs are 100% donor dominant.
This begs the question… just how much influence can a recipient site have on a hair?
Apparently a lot. And here is where things get more interesting.
Balding human hairs can regenerate when transplanted onto a mouse
A 2002 study from the Orentreich Foundation for the Advancement of Science (yes, the very same Dr. Orentreich) transplanted both balding and non-balding human hairs into the backs of mice. 22 weeks later, what were the findings?
The balding human hairs had regenerated just as well as the healthy non-balding hairs… and this regeneration happened in a single hair cycle.
In fact, those balding hairs continued thickening through the duration of the study… whereas the non-balding hairs, for reasons unknown, plateaued after 17 weeks.
How is that possible? Aren’t balding human scalp hairs supposed to continue to thin – like they did in that case study of the 29-year old whose balding scalp hairs were transplanted to his forearm?
Again, the researchers couldn’t explain their results with 100% certainty. They thought the regeneration might be due to lower androgen levels in mice – similar to how finasteride (an androgen reducer) might improve hair loss in men. But the hairs regrew just as well on male (higher androgen) and female (lower androgen) mice — which they couldn’t explain.
Even odder – the balding hairs regenerated in a single hair cycle – much faster than hair recoveries seen from finasteride in humans. To the researchers, this suggested the influence of non-androgenic factors in the recovery of those hairs. Yet that was as far as they could extrapolate.
Again, this contradicts the original hair transplant studies. Balding hair follicles should keep thinning no matter where they’re placed. Except this study shows that’s not always true.
So, are there any other examples of hair follicle regeneration from environmental influence?
Yes. And this next study even gives us insights as to what may explain the discrepancy in newer findings versus the original hair transplantation studies.
Hair-plucking increases hair follicle proliferation five-fold… but only if many hairs are plucked from a small region
In 2015, researchers wanted to see if hair follicles could communicate with each other to coordinate behaviors – like making new hair follicles. So they set up a test…
They plucked 200 hairs from the backs of mice… but did so while controlling for the diameter of a plucking region. In some cases, 200 hairs were plucked in a 2.4mm region. In other cases, 200 hairs were plucked from an 8mm region. The smaller the region, the higher-density the plucking – and vice-versa.
The goal: to see if hair follicle behavior changed on how closely hairs were plucked from one another. So they measured hair growth over the next several weeks.
The results were fascinating.
With low-density plucking, hair follicles either didn’t grow back at all… or grew back to its normal pre-plucking density. That’s what we would expect to happen.
But with higher-density plucking, additional hair follicles were created… to the tune of a five-fold increase.
What’s more interesting is why this happened. The researchers theorized that higher-density plucking created more inflammatory signaling, which led to more cross-communication between hair follicles directly next to each other, which signaled to hair follicles to start regenerating – regardless of whether they’d been plucked. The end-result: a huge increase in hair.
What does this show? Two things…
- A hair follicle’s immediate environment can influence its ability to grow. We saw this in changing the hair’s environment (i.e., transplanting balding human hair onto a mouse)… and by augmenting that environment (i.e. plucking many hairs from a small region). In both cases, hair recovery ensued.
- The immediate environment that hair follicles use to cross-communicate can be very small.
Let’s elaborate on that second point. For reference, those plucking “zones” the investigators used ranged from 2.4mm to 8mm – yet researchers only observed hair follicle proliferation in plucking zones of 4mm and smaller.
Now let’s reflect back to those original hair transplantation studies.
These studies used skin punch biopsies of 6mm to 12mm – each of which contained up to several dozen hair follicles. Yet our inferences from those transplantation studies were that scalp hair follicles are donor dominant – they retain their characteristics wherever they are transplanted.
Do you see the irony?
We’re saying that hair follicles can coordinate to make new hair follicles across distances of 4mm distances or smaller… while simultaneously saying that scalp hair follicles aren’t influenced by the environment, as demonstrated by transplanting 6-12mm chunks of skin containing dozens of hairs and watching them not change their behavior.
So… does the amount of tissue transferred alongside hair follicles influence hair transplant results?
This is actually the second question we need to answer in order to refute the scalp tension hypothesis. And while nobody’s actually fully answered this question… preliminary evidence suggests that yes -the amount of tissue transferred alongside a hair follicle transplant does influence its survival.
2. Does the success rate of a hair transplant depend on how much adjacent tissue is transferred alongside the hair follicles?
In both Orentreich’s original study and the primate transplant study, hairs from skin punch biopsies of 6-12mm retained their original characteristics when transplanted into balding regions – and for 2.5 to 8 years.
But again, these punch biopsies contained dozens of hair follicles and their surrounding tissue. As we’ve just learned, surrounding hair follicles and tissues communicate with each other to react to environmental influences.
But do these tissues also help hair follicles maintain their original growth characteristics?
In other words, if we strip away these tissues, isolate a hair follicle unit to just a single hair follicle, and then transplant that into a balding region, what happens?
Interestingly, those hair follicles don’t always survive.
Hair follicle transplant survival rates decrease if individual hairs – rather than full hair follicle units – are transplanted
This is exactly what these researchers discovered when investigating hair transplant survival rates for individual hairs versus hair follicle “clusters” – known as hair follicle units.
Specifically, these researchers were exploring a new hair transplantation technique known as follicular unit extracts (or FUE). This is when, rather than taking larger punch biopsies or “strips” of skin containing hundreds of hair follicles – a surgeon instead takes a series of 0.6-1.2mm “punches” containing individual hair follicle units (usually 4-8 hairs) spread throughout the donor area. This allows for less scarring from a transplant.
Their findings: if a hair follicle is separated from its follicular “unit” – its survival rate decreases. In fact, single hair follicles are 25% more likely not to survive… at least in the 26-week period of the study.
In the words of the study:
“Extremely high survival rates of micrografts are obtainable by transplanting intact follicular clumps with protective tissue around the micrograft, and preserving the follicular clump’s sebaceous gland. These survival rates were not achieved when micrografts were produced by splitting individual hairs away from a naturally occurring follicular clump.”
Do hair transplantations always last forever?
With 6-12 punch biopsies and “strip” transplantations, these hairs certainly last for a very long time. Certainly long enough to validate the surgery (if you’re considering doing it).
But as with these techniques – and with newer techniques, like follicular unit extractions (FUE) – survival rates seem to depend on how much connective tissue is also transplanted alongside the hair follicle, and if a hair follicle unit is transferred altogether.
I haven’t found any studies investigating the long-term efficacy of FUE transplantations. But it seems like there’s enough preliminary evidence to suggest that the less surrounding tissue transplanted alongside the hair, the less successful the hair transplant.
In FUE literature reviews, researchers address these concerns by acknowledging that, over time, even donor regions of a scalp can still succumb to miniaturization from pattern hair loss. In other words, over the years, the loss of transplanted hairs is perhaps to be expected.
“While the follicular units in the optimal donor area of the occipital and parietal scalp are ″relatively″ protected from androgenetic hair loss, even those follicular units may be somewhat affected with time.”
For the record, this is absolutely true. In many cases of androgenic alopecia, regions beyond the galea aponeurotica will succumb to hair follicle miniaturization – especially in advanced stages. And the truth is that regardless of an FUT or FUE procedure, hair follicle survivability is likely dependent, in part, on how much tissue the surgeon trims away from each follicle prior to transplanting it.
Additionally, as more surgeons transition to FUE, many now mandate to their patients to take finasteride. In fact, a lot of surgeons won’t even perform FUE surgery unless their patient agrees to this.
Obviously, this is to the interest of the patient. Finasteride is incredibly powerful at stopping hair loss – and as more FUE patients commit to taking it, it will improve their odds of their hair transplant sticking and looking great for years to come.
At the same time, mandating finasteride use post-FUE transplantations will make it harder to grasp how individually transplanted hair follicle units (and sometimes, just single hair follicles) behave over decades in a balding environment. The FUE studies bank on these follicles behaving the same way as they did in the original hair transplantation studies. But again, I’m not sure this is the case.
Perhaps unsurprisingly, a lot of readers here who did an FUE and then stopped taking finasteride have reported that their transplanted hairs are falling out. That’s concerning – especially as these readers have also reported that the regions from where those transplanted hairs were taken have not had any noticeable miniaturization.
While many surgeons claim this only happens if a transplanted hair is taken too close to the vertex (where thinning might later occur) – this seems to happen far too often to explain all cases.
Again, here’s a 2013 literature review suggesting these newer, smaller “micrograft” techniques might not match up to Orentreich’s hair transplant findings with larger punch biopsies…
“Micrograft survival rates in hair transplantation have been frequently described in private conversations by hair transplant doctors as variable at best. References in medical literature may grossly underestimate the prevalence and magnitude of poor growth. This is probably because most hair transplant surgeons are concerned that publication of a significant incidence of poor growth would reflect negatively on their practice.”
In my conversations with other AGA researchers, a few have stated – contrary to popular belief – that transplanted hairs do thin. There’s even a hypothesis that transplanted hairs simply restart their “balding clock” post-transplantation – meaning that in 5, 15, or 25 years, we can expect transplants to start thinning as well.
Only time will tell.
In any case, there at least appears preliminary evidence that a hair follicle’s surrounding environment influences its growth characteristics… that this includes both balding and non-balding scalp hairs… and that hair transplantation success might depend on how much of the surrounding environment is transplanted along with the hair.
Do transplanted hairs experience the same “tensile” environment as recipient site hairs?
Another thing we’d need to confirm for hair transplantations to refute the scalp tension hypothesis is that after an operation, transplanted hairs experience the same tension as the recipient site hairs.
Unfortunately, this hasn’t yet been studied. But based on what has been studied, we can infer that this might or might not be the case.
Interestingly, in that eight-year transplant study on balding primates, investigators biopsied the transplanted skin periodically after the procedure – to see what was going on underneath the skin.
They found that after one week, transplanted tissues fused with surrounding tissues. Soon after, the transplanted hairs fell out, and then began regrowing a number of weeks later as underlying tissue began to merge toward the transplanted tissue. At four months, the underlying transplant tissue looked nearly identical to the surrounding tissues – minus the larger hairs.
This might suggest that these hairs do experience the same tension as surrounding hairs, but it’s really hard to say. What isn’t studied here is the differences in tensile readouts between transplanted hair follicles and their surrounding environments. As another researcher mentioned in his critique of the balding scalp hair-to-forearm transplant study we mentioned earlier…
“…According to the approach of the present paper, it would be necessary to know the strain supported by the forearm skin and to realize that the hair follicles close to receding hairline have already started a countdown toward the miniaturization, but not the occipital follicles. In hair transplantation, the grafted follicles start a new “balding clock,” but hair growth would be guaranteed for many years even without preventive pharmacotherapy.”
What also isn’t studied is the role of epigenetics in these transplants – or in other words, the changes in gene expression pre- and post- hair transplantation. When these transplant studies were conducted, epigenetics wasn’t even a field of scientific study. So again, there are just a lot of unknowns here… so we need to exercise caution with how we interpret these studies and apply implications.
In any case, we can now summarize why hair transplantation successes might not refute the scalp tension-AGA hypothesis.
Summary: why hair transplants might not refute the scalp tension-hair loss theory
Hair transplantations are overwhelmingly successful. Early transplant studies suggested that scalp hairs transplanted into balding scalp environments retain their original characteristics and keep growing forever – a concept known as donor dominance. Many people use these studies to refute the scalp tension hypothesis – and with good reason.
At the same time, relieving scalp tension appears to improve androgenic alopecia (for references, please see the first article). So we should probably try to make sense of these paradoxical findings.
Reevaluating the original hair transplantation studies, we see that the investigators transplanted 6-12mm skin punch biopsies containing dozens of hair follicles per transplant. This might create a few problems when trying to use these studies as evidence against the scalp tightness-AGA theory:
- Studies show hair follicles communicate with each other to maintain or increase hair follicle counts in regions of 4mm and smaller. Thus, we can’t conclude that baldness is determined within each hair follicle if these transplant studies use punch biopsies large enough to allow for inter-follicular communication.
- There’s preliminary evidence that as we trim away surrounding tissues, hair follicle transplantation survival rates decrease. This is most obvious in FUE micrograft studies of single hair follicles – where researchers separate a hair follicle from its hair follicle unit, and then observe worse survival rates post-transplantation into balding regions.
- Moreover, recent studies demonstrate that human scalp hair follicles do take on characteristics of their recipient sites… and that balding human hairs can regenerate in a single hair cycle if transplanted onto the back of a mouse. In other words, human scalp hairs are susceptible to their environment – which refutes aspects of Orentreich’s original findings.
These findings, along with many anecdotes from patients with failed FUT and FUE transplants (despite no miniaturization observed from where the hairs were transplanted), have led some AGA researchers to conclude transplanted hair follicles might eventually thin. Rather, it’s just that after transplantation, their “balding clocks” are set back to zero… and thus we might need to wait 5, 15, or 25 years to begin to see the effects.
Again, this is not to say hair transplants aren’t long-lasting. In most cases, they certainly are. It’s just to say that there’s evidence that transplanted hairs might also be susceptible to AGA with time… and that recipient sites of transplanted balding scalps have a bigger influence on their growth than we initially thought.
How can transplanted hairs grow in fibrotic scalp environments?
According to some models of the scalp tension hypothesis, fibrosis (or scar tissue) is a rate-limiting factor for hair recovery. This has led some to ask, “If regular hair can’t grow in fibrotic tissues, how come transplanted hairs can?”
Interestingly, we can use the findings of a recent (and fascinating) study to help answer this question. It was conducted, in part, by one of the biggest names in hair loss research: Dr. George Cotsarelis.
Dr. Cotsarelis and his team wanted to understand the role of the hair follicle during wound-healing. It has been long understood that where there is scar tissue, hair cannot grow. We see this in burns, scleroderma patients, and in advanced stages of androgenic alopecia (pattern hair loss) where scar tissue is present in skin tissues, thus preventing the proliferation of hair follicles (and thereby hair growth).
What Cotsarelis and his researchers discovered: if we can regenerate a hair follicle first, that hair follicle will begin to signal to its surrounding tissues to regenerate other cell types normally lost to scar tissue – like adipose tissue (or subcutaneous fat).
What does this have to do with hair transplant survival rates? Well, think about it:
- In AGA, fibrosis (scar tissues) restricts hair follicle growth space, leading to hair loss.
- Hair transplants take hair follicle units from the backs of our scalps and transplant them into balding areas where there is scar tissues
- In doing so, they provide scarred tissues with newer, healthy hair – and in a way, “force” the regeneration process of nearby tissue – thus partially resolving fibrosis in surrounding tissues and allowing for the transplanted hairs to grow.
Interestingly, this might be why some hair transplant surgeries observe transplant survival rates of over 100%. This was originally believed to be the result of hidden telogen (resting) hairs moved during the hair transplant. Now it’s possible that these extra hairs are actually bald vellus hairs regenerating as a result of cellular signaling from the transplanted hairs.
In fact, this study might not only explain why transplanted scalp hairs survive in balding environments… but also the mechanisms behind why they reset the baldness clock – if we choose to believe that concept at all.
Final remarks: scalp tension and hair transplants
The scalp tension-AGA hypothesis is far from proven, but it’s also far from debunked.
At face-value, older hair transplantation studies refuted the scalp tension theory and led researchers to believe that hair follicle miniaturization was programmed within the hair follicle itself – not its environment.
However, these transplant studies were conducted using 6-12mm skin punch biopsies. A 6-12mm biopsy contains dozens of hair follicles and a lot of surrounding tissues. That’s a far cry from a single hair follicle. Resultantly, 6-12mm punch biopsies don’t really tell us much about what happens if we transplant an individual hair follicle into a balding region – absent of its surrounding tissues.
New research suggests that surrounding tissues do influence the regulation and proliferation of the hair follicles they support. And interestingly, survival rates for transplanted hairs decrease as we trim away surrounding tissues and transplant just singular instead of entire hair follicle units (4-8 hairs), strips, or punch biopsies.
This suggests the conclusions of the hair transplant studies from 1959-1982 actually should attribute more of their success to the surrounding tissues transplanted alongside the hair follicle – and the fact that entire hair follicle units were transferred (not just single hairs) – which likely allowed these tissues to maintain follicular communication and regular their growth and proliferation even in their newly transplanted environment.
Given all of this, and the potential variability in success with FUE transplants, several AGA researchers now believe that transplanted hairs simply reset on a balding clock – and that given enough time, they eventually will thin.
On top of that, newer studies show that healthy transplanted hair follicles actually help to signal to surrounding tissues to regenerate – just explaining why they can proliferate in balding regions (or maybe even support the proliferation of surrounding balding hairs).
All of this isn’t to say that the scalp tension hypothesis is irrefutable. On a personal level, I don’t think that scalp tension explains all aspects of AGA (more on this later). This is just to say that hair transplantation studies don’t necessarily refute the scalp tightness theory – especially in light of newer evidence.
At the end of the day, relieving scalp tension – either through botulinum toxin injections or mechanical offloading – seems to improve AGA outcomes. So if scalp tension doesn’t contribute to pattern hair loss… relieving scalp tension seems to still help regrow hair.
Is the scalp tension theory true? I don’t know. Maybe. Maybe not. But I don’t think these original hair transplant studies refute it. And in the next article, we’ll discuss where this “scalp tension” might originate.
Rob English is a researcher, medical editor, and the founder of perfecthairhealth.com. He acts as a peer reviewer for scholarly journals and has published five peer-reviewed papers on androgenic alopecia. He writes regularly about the science behind hair loss (and hair growth). Feel free to browse his long-form articles and publications throughout this site.