Read time: 15 minutes
What Causes Hair Loss?
If you ever google’d “what causes hair loss?”, you’ll find thousands of results saying hair loss is due to…
- Genetics
- DHT (dihydrotestosterone)
- High testosterone
…and a million other one-liner answers.
The reality? These statements are too simple to be right or wrong. For instance:
Yes, our genes might predispose us to hair loss, but gene expression likely matters more than genes alone.
Yes, DHT (a hormone made from testosterone) is linked to hair loss… But only one kind of DHT: scalp tissue DHT. Paradoxically, serum (blood) DHT is sometimes linked to lower levels of scalp hair loss, and body tissue DHT encourages body hair growth.
Yes, hair loss occurs in high-testosterone men… But it also occurs in low-testosterone men. What actually matters is the amount of testosterone converting into scalp tissue DHT – and why.
So how do we distinguish hair loss fact from fiction? As one reader recently wrote in…
“I have been losing my hair for about ten years and I don’t really know where to start because of the overload of information online. What do you recommend are the first steps I can take?”
Unfortunately, there’s no easy answer. So my #1 recommendation is: get informed.
Learn Everything You Can About Hair Loss Science
Don’t just read summary articles. Read peer-reviewed studies. And don’t just read abstracts. Read full papers. Don’t know a term? Look it up. Have a question? Email the author. You’d be surprised how many will get back to you.
The more you know, the better informed you are, the quicker you can sort out the misinformation.
Of course, not everyone can spend years of their life reading pubmed journals. And not everyone can access the full texts from studies. That’s why I wrote this article – to share some of my ideas on hair loss pathology, formulated over the years.
Inside This Article: The Causes Of Hair Loss Mapped Into A Flowchart
This a long post. The goals are to simplify some elements of hair loss science so we can better understand the benefits (and limitations) of treatments, as well as some angles of attack for pattern hair loss. If you have any questions, please reach out in the comments.
Important Note: since writing article, my views on pattern hair loss have evolved. While the following article helps to clarify two rate-limiting recovery factors in pattern hair loss, it fails to dive deep enough into the genetic predisposition of AGA, its potential relationship to mechanotransduction, a concrete explanation for the DHT paradox, and a rationale for the patterning of hair thinning in men and women.
Rather than continuously revise this article and distill what is (very) complex science into lay terms, I instead decided to write a manuscript and submit these ideas to peer-review. The paper was accepted in late 2017. You can read it in full right here, along with a lay person’s breakdown of (some of) its arguments here.
Otherwise, please consider this article a starting point to uncovering additional factors (beyond DHT) involved in androgenic alopecia. And, please disregard my original emphasis on diet, lifestyle, and testosterone:estrogen ratios. While these factors are certainly linked to systemic inflammation and non-androgenic forms of hair loss, the sources of inflammation in AGA are a little less clear, and likely less connected to these factors than I originally implied.
Finally, here is a more updated overview: Androgenic alopecia: its causes, treatments, and unknowns.
Tracing The Causes Of Hair Loss: Where To Begin?
Let’s start with what our fingers feel and our eyes see: our thinning hair and the skin underneath it.
A Close-Up Of The Balding Scalp
Where is your hair thinning? Temples? Vertex? All over? Using your hands, feel the thinning areas of your scalp. Then feel your non-thinning areas (the sides or back of your head).
Notice anything? In balding sites, our skin feels thicker, less pliable, and significantly less elastic. Touch the green part of your scalp, then the blue. Feel the difference.
Balding Regions Have Thicker, Tighter Skin
Next, grab a mirror and look at your head. Do you see any visual differences in your balding versus non-balding regions?
In balding areas, many men’s scalps have a certain “shine” to them. You might see this too. In advanced stages, some balding regions can even look swollen.
Balding Regions Are Shinier, More Swollen
Why do balding parts of the scalp feel tighter, thicker, and look shinier and more swollen?
Your balding scalp is tighter, thicker, and shinier because of an overproduction of something called collagen.
Collagen is the fibrous protein that makes up our connective tissues, like our skin. If you ever get a small paper cut, your skin cells make new collagen to repair the wound and make the skin as smooth as it used to be. But if we cut our skin too deeply, our skin can make too much collagen.
But it’s not just too much collagen. It’s disorganized collagen cross-hatchings. This leads to imperfect healing and scar tissue.
Balding Skin Is Tighter, Thicker, And Shinier Due To Excess (Disorganized) Collagen
Interestingly, men with pattern hair loss have four times the amount of collagen fibers at the temples and vertex than men with no hair loss at all. What does that indicate? Balding skin is ridden with scar tissue.
Disorganized (Excess) Collagen Is Also Called Fibrosis
There’s another word to describe the disorganized, over-accumulation of collagen: fibrosis. And while our balding scalps are wrought with excess collagen, our thinning follicles are also surrounded by it! This is called perifollicular fibrosis.
In other words… where there’s hair loss, there’s fibrosis. But does fibrosis cause hair loss?
We can find our answer by studying a rare autoimmune condition that makes people over accumulate collagen and fibrosis. It’s called scleroderma.
The Scleroderma-Fibrosis-Hair Loss Connection
In scleroderma, the body starts to overproduce collagen – sometimes in the lungs, hands, and even the scalp. Regardless of the location, this process results in the same visual symptoms we see in balding scalps: tighter, thicker, shinier-looking skin.
Just look at this photo of a scleroderma sufferers’ hands, and then this photo of a hair transplant patient’s scalp.
Notice the shine around the knuckles and the shine across the top of the scalp… It’s the same skin quality. Same shine, same thickening, same swelling.
But most interestingly, for those who develop scleroderma in the scalp, hair loss soon follows.
That’s a critical piece of information. It confirms that excess collagen and fibrosis occur before hair loss starts. They precede hair thinning. Excess collagen and fibrosis accumulate first, then hair loss comes later.
Scalp Fibrosis Develops Before Hair Loss
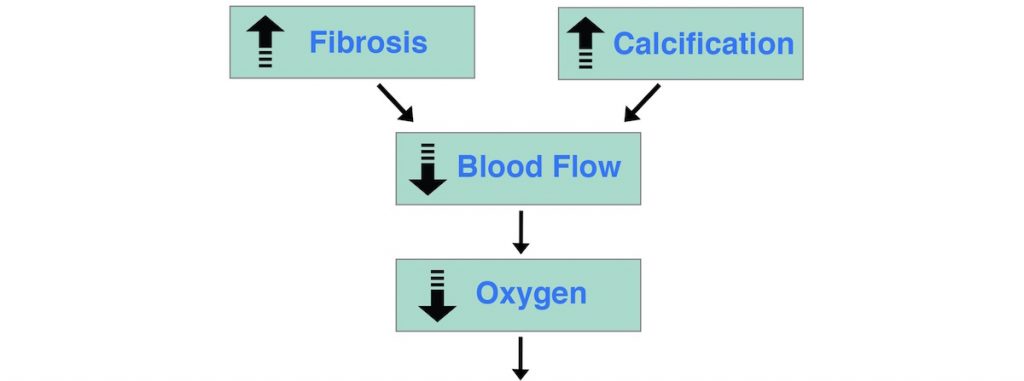
Knowing this, we can begin to build our flowchart:
But how exactly does disorganized, excess collagen (or fibrosis) lead to hair loss?
Fibrosis Restricts Blood Flow To Our Hair Follicles
Body tissues wrought with excess collagen and fibrosis also have lower blood flow. This is even documented in balding regions – blood flow is restricted in thinning areas of our scalps. The more collagen and fibrosis, the more blood flow is restricted.
Knowing this, it’s no surprise that nearly all scleroderma sufferers also have poor circulation of the extremities (hands, feet, and head). Poorer circulation, less blood flow… But less blood flow also means less oxygen.
Lower Blood Flow Lowers Your Tissue’s Oxygen Supply
Blood carries oxygen to our tissues. If our tissues have lower blood flow, they also have lower oxygen levels. Low tissue oxygen is also known as hypoxia. Studies confirm that balding scalp regions are hypoxic.
If a tissue is chronically suffering from low blood flow and low oxygen, hair cannot grow.
In one study, men’s balding regions had just 60% the oxygen levels of non-balding areas. Men with no hair loss had oxygen levels nearly the same all across their entire scalp.
Knowing this, we’ve just added to our flowchart. Excess collagen (fibrosis) decreases blood flow and oxygen, and in doing so, “chokes out” our hair follicles. This leads to hair loss.
Now, are there any other conditions in a balding scalp that might also decrease blood flow and thereby oxygen to our follicles?
Yes. Beneath our scalp skin is another contributing factor: arterial calcification.
Our Scalps Have Become Partially Calcified
It’s not just fibrosis that reduces blood flow and oxygen to our hair. In balding areas, the blood vessels that indirectly support our follicles – in the lower layers of the scalp – may have also become calcified!
Dr. Frederick Hoelzel in the American Medical Association published the connection between scalp calcification, restricted blood flow, and hair loss over 70 years ago. When removing the brains of cadavers, he discovered:
“Baldness occurred in persons in whom calcification of the skull bones apparently had not only firmly knitted the cranial sutures but also closed or narrowed various small foramens through which blood vessels pass most prominently in persons with a luxuriant crop of hair.”
For the layperson – in balding regions, our scalp bones and blood vessels supporting the follicles are calcified. If an artery is calcified, blood flow is significantly restricted.
What Is Calcification?
According to medical experts, calcification is “when calcium builds up in places where it doesn’t usually appear, like the coronary arteries or brain.”
Since elderly people often have more calcification, researchers once thought this process was a part of normal aging. But it turns out the relationship between age and calcification doesn’t really exist. Calcification doesn’t have to increase with age. It can be rampant in young adults and nearly absent in older ones.
And finally, it’s also important to note that calcification is not necessarily caused by a calcium-rich diet.
So back to our flowchart. Does calcification cause fibrosis?
Probably not. Most research suggests that calcification and fibrosis can occur in the same areas, but are likely independent of each other. And while some scleroderma patients also suffer from soft tissue calcification, others just suffer from an overproduction of collagen. So calcification does not have to happen before fibrosis and vice-versa.
Knowing this, we’re ready to add calcification into our flowchart. For simplicity’s sake, we’ll remove the visuals describing a balding scalp – the “thicker, tighter, shinier skin.”
Now let’s start tracing this chart backwards. We’ve gone as far as calcification and fibrosis. So what triggers both?
Calcification And Fibrosis Precede Hair Loss…
…But What Causes Calcification And Fibrosis?
We can get an idea of what might be causing these conditions if we look at the people most likely to develop arterial calcification and fibrosis: men.
Men are almost twice as likely as women to develop calcified arterial lesions. Why is that? Researchers have long suspected that androgens might be to blame. Read: testosterone and DHT – or dihydrotestosterone.
Why is this so interesting?
Well, most doctors agree that DHT causes hair loss… But none actually know how DHT causes hair loss. If DHT triggers calcification and fibrosis, this explains how DHT causes hair loss. But to confirm this, we need to know if androgens (like DHT) actually precede arterial calcification and fibrosis.
The DHT-Calcification-Fibrosis Connection
Does DHT Cause Calcification And Fibrosis?
Research here is mixed.
On the one hand, men and women who take androgens (steroids) significantly increase their risk of arterial calcification. And in mice, DHT and testosterone injections increase arterial calcification lesions by 200-400%. The more DHT or testosterone injected, the greater the calcification. That’s a pretty strong case that androgens cause calcification.
But paradoxically, in studies done in test tubes (outside of our bodies), increased androgens don’t cause calcification. In these tests, androgens protect against calcification.
This suggests two things:
- Androgens alone don’t cause calcification
- The test tube studies are missing at least one variable. It must be that increased androgens plus at least one “mystery variable” leads to calcification – but not androgens by themselves.
DHT is the main androgen associated with pattern hair loss. But we also know that DHT alone doesn’t cause calcification and fibrosis… So DHT by itself can’t be the problem.
What does this suggest?
In the scalp, increased DHT plus these “mystery variables” precede both calcification and fibrosis. Knowing this, here’s our new flowchart:
So what could these mystery variables be?
Well, there are two. The first is an increase in androgen receptors. The second is an imbalance of calcification regulators. And explaining both are a bit of a mouthful. So bear with me.
A Crash Course On DHT, Androgen Receptors, And Calcification Regulators
We know that androgens alone don’t cause calcification, and that in the body, androgens must be interacting with other variables to cause calcification and fibrosis. So, what are those variables?
It appears there are two. And in 2016, researchers finally confirmed the first one: androgen receptors.
What Is An Androgen Receptor?
An androgen receptor (AR) is the place inside a cell where androgens – like testosterone and DHT – attach themselves. Think of an androgen receptor (AR) like the landing pad for DHT. Without its landing pad, DHT doesn’t bind to the cell.
Here’s a visual. This is a cell, and the yellow puzzle pieces (labeled AR) are androgen receptors:
(source)
Androgen receptors aren’t always active. They typically turn on in the presence of DHT or testosterone, then turn off when these hormones aren’t around.
The Connection Between Increased DHT And Increased Androgen Receptors
In our scalp tissues, increased androgens turn on more androgen receptors, and together, the increased DHT plus the increased androgen receptors results in calcification. Both DHT and androgen receptors must increase (not just one) for calcification to occur.
Interestingly, DHT plus androgen receptors also increase fibrosis in heart cells.
In other words, increased DHT + increased androgen receptors precede both calcification and fibrosis.
But here’s where things get tricky… Increased androgen receptors aren’t the only other variable. We know this because of DHT’s biggest paradox:
That means that in our hairy facial and body tissues, calcification and fibrosis don’t occur. Why? Because in our bodies and face, increased DHT instead encourages hair growth – just the opposite of our scalps.
If our flowchart is accurate, this means that in the body and face, when DHT increases, androgen receptors must not increase. Otherwise, our body and facial tissues would also calcify, and hair wouldn’t grow.
But as it turns out, both balding scalps and hair-bearing body and facial tissues have increased DHT and increased androgen receptors… Yet hairy body and facial parts aren’t calcified or filled with fibrosis.
What does all of this mean?
In addition to DHT and androgen receptors, another factor must also be causing calcification and fibrosis. Either something is protecting our body and face from fibrosis and calcification, or something is causing both to happen in our scalps.
Taking this into account, here’s our new flowchart:
So, what is this new mystery variable? There are several contenders, but diving into all of them would turn this already-monstrous post into a full-blown book.
The reality is, we don’t yet know for sure.
The reason why: 99% of researchers still abide to the DHT-sensitivity argument. They say that “genetics” makes our hair follicles more sensitive to DHT, and that for unknown reasons, DHT accumulates in the scalp and eventually causes hair loss. To my knowledge, there are no current studies even exploring scalp DHT’s connection to calcification (even though when we look at broader research, the connection seems obvious).
On top of that, researchers only recently confirmed (in 2016!) that both an increase in androgens and androgen receptors are needed to cause calcification, not just one. This discovery came from cardiovascular researchers and not hair loss researchers. These fields don’t really talk to each other. Neither is very aware of the other’s work. As a result, our third mystery variable remains a mystery.
But even still, we can make a very strong case for what this variable could be.
Uncovering The New Mystery Variable
Here’s what we know: if we inject regular mice with DHT, they develop calcification. But if we inject DHT into mice who can’t produce androgen receptors, no calcification occurs. Why?
Let’s start by looking at the “engineered” mice who can’t express androgen receptors. When they receive DHT, their bodies respond by…
- Activating proteins associated with calcification inhibition
- Deactivating proteins associated with calcification induction
In other words, these engineered mice turn on proteins that suppress calcification, and turn off proteins that encourage calcium buildup. The end result: no calcification.
So how do the regular mice – the ones with androgen receptors – respond to a DHT injection? Just the opposite. When these mice receive DHT, their bodies…
- Turn on proteins that encourage calcium buildup
- Turn off proteins that usually suppress calcium buildup
The result? Calcified arteries.
This is important. Surrounding our bodies and facial hair, we don’t develop the same calcification or fibrosis that we see in balding regions of the scalp. The same isn’t true for our scalp hair. This suggests one thing:
Our new mystery variable is likely, among other things, an imbalance of calcification regulators.
What Are Calcification Regulators?
Calcification regulators are a set of (mostly) proteins with many names and functions. They regulate whether your tissues accumulate or release calcium. We won’t dive into each of them, but if you want to do more research, here are some examples.
For the calcification inhibitors, there’s…
- fetuin-A
- matrix gla protein
- osteopontin
- osteoprotegerin
- and dozens of others
For the calcification inducers, there’s…
- prostaglandin d2
- transforming growth factor beta 1
- bone morphogenetic protein 2
- bone morphogenetic protein 4
- alkaline phosphatase
- and many more
Not surprisingly, studies have linked each of these “inducers” to hair loss… but no one’s yet identified their relationships to calcification.
The Hair Loss Triple Threat: Increased DHT + Increased Androgen Receptors + Imbalanced Calcification Regulators
Remember, we need three factors for calcification and fibrosis to occur: increased DHT, increased androgen receptors, plus an imbalance of calcification regulators.
This new flowchart checks out against all the available evidence, including the DHT paradox:
A Quick Recap:
- Androgen receptors (AR) are the places inside our cells where androgens – like DHT – attach themselves. Androgen receptors often turn on or off depending on whether androgens are near. In order for calcification and fibrosis to occur, we need an increase in androgens (DHT) and an increase in androgen receptors.
- At the same time, there must also be an imbalance of calcification regulators. Calcification regulators are a set of molecules, enzymes, and proteins that control whether our tissues store calcium. There are two categories: calcification inducers (promoters) or calcification inhibitors (suppressors). If our body tissues activate too many inducers and too few inhibitors, calcification will accumulate.
- Imbalanced calcification regulators explain the DHT paradox – or why DHT encourages hair loss in the scalp but hair growth in the body and face. These regulators stay balanced in hair-bearing body and facial tissues. These don’t calcify. But in the scalp, more inducers than inhibitors activate. The result? Scalp calcification and fibrosis.
We need a combination of all three factors to induce calcification and fibrosis:
- Increased DHT
- Increased androgen receptors
- Imbalanced calcification regulators
Now let’s start tracing this flowchart backwards again.
What could possibly trigger increased DHT, increased androgen receptors, and imbalanced calcification regulators simultaneously?
There are likely two main causes. The first is chronic inflammation. The second is a hormonal imbalance.
Cause #1: Chronic Inflammation
What Is Inflammation?
Inflammation is our bodies’ natural reaction to stressors, like an injury, infection, or toxic chemicals.
For instance, say we stub our toe on a door. Our bodies recognize this injury as a “threat”. Then they activate enzymes, proteins, and hormones to kickstart the healing process. These molecules assess the damage, then determine how much our toe should swell (the pro-inflammatory response) and when to activate repair proteins (the anti-inflammatory response). This is all natural, normal, and healthy.
Chronic inflammation is not healthy. This is when inflammation never resolves – like a virus that won’t go away, or an ulcer that won’t heal. In these cases, inflammation is always present, so our tissues never fully repair. This is the type of inflammation associated with autoimmunity and cancer – and often leads to scarring (read: fibrosis).
Interestingly, increased DHT isn’t just found in balding scalps… It’s also found in inflamed body tissues. There’s even evidence that DHT actually helps regulate inflammation, and that in some tissues, DHT is anti-inflammatory.
This suggests that increased DHT is a part of the inflammatory process. DHT binds to tissues after inflammation occurs. And in our balding regions, if DHT is chronically elevated, our scalps are also probably chronically inflamed.
When we reflect on the causes of calcification and fibrosis, this makes sense. Studies show calcification and fibrosis are both the end-result of chronic inflammation.
Chronic inflammation is the gun. The DHT-AR-calcification regulator imbalance is the trigger.
But there’s one more “gun” that fires calcification and fibrosis… A hormonal imbalance.
Cause #2: Hormonal Imbalance
Hair loss is closely connected to a hormonal imbalance. Specifically, our testosterone:estrogen ratio.
In women, thinning hair has been linked to higher testosterone:estrogen ratios than non-thinning women. In younger balding men, elevated estrogen levels are also common.
But this is just an association… Where does our T:E ratio fall into our flowchart? Evidence shows that this imbalance happens before calcification and fibrosis.
The T:E-Calcification Connection
Our T:E ratio may actually control which calcification regulators our bodies activate.
Remember: if too many calcification inducers and too few calcification inhibitors are active, calcification occurs.
Our body’s T:E ratio is something that helps “regulate” our calcification regulators. If our T:E ratio is imbalanced, we’re at a higher risk of calcification.
This explains why an imbalanced T:E ratio is so strongly associated with heart disease. In men, lower testosterone levels are associated with higher rates of calcification and stroke. Low testosterone men have a near two-fold increase risk in morbidity. They also suffer from higher arterial stiffness (think: fibrosis). Finally, men with higher estrogen levels are also more likely to develop arterial calcification.
In women, low estrogen levels are associated with higher arterial calcification. Women with polycystic ovary syndrome and high testosterone also have higher rates of arterial calcification. The same is true for women receiving testosterone injections after menopause – the time when their estrogen levels plummet.
So let’s add chronic inflammation and an imbalanced T:E ratio to our flowchart:
Now for one final question…
What Triggers Chronic Inflammation And A Testosterone:Estrogen Imbalance?
While there are thousands of factors that contribute to chronic inflammation, an imbalanced T:E ratio, and the conditions that cascade into hair loss, there are four big ones…
Our diet, lifestyle, microbiome, and scalp environment.
For purposes of this article, we’re not going to trace these pillars back any further. The new book covers each pillar in detail – its triggers and what to do about them. For now, here’s the foundation of our hair loss flowchart.
The Master Hair Loss Flowchart
This chart is logic-checked against the scientific literature on DHT, hair loss, calcification, fibrosis, and everything in between. It’s a pretty far step from all the one-line answers doctors tell you, like “DHT causes hair loss” or, “You lose hair when you’re stressed.”
But most importantly, this chart is a tool that allows us to evaluate hair loss treatments. So let’s start using it!
Using The Master Flowchart To Evaluate Hair Loss Drugs
Our flowchart explains not only why a drug like Minoxidil is relatively ineffective at reversing hair loss, but also why Finasteride might be great at stopping hair loss but less effective at regrowing hair. (Note: for a quick overview of Minoxidil and Finasteride, read this).
Minoxidil Versus Our Flowchart
Minoxidil works by providing more blood flow to the follicles. Where is “blood flow” implicated on our flowchart?
Almost right at the bottom (after calcification and fibrosis).
Remember: calcification and fibrosis are chronic, progressive conditions. This means that they don’t go away on their own and they tend to get worse over time.
Increasing blood flow helps our follicles temporarily. But because Minoxidil doesn’t reverse the calcified, fibrotic condition of our scalps, this effect only provides a temporary boost to our hair follicles.
As calcification and fibrosis worsen, Minoxidil’s effectiveness fades.
Finasteride Versus Our Flowchart
Finasteride works by preventing the conversion of free testosterone into DHT. It prevents tissue DHT from accumulating in our scalps. Where does this take place on our flowchart?
Right before calcification and fibrosis.
Since Finasteride reduces DHT in the scalp, it helps stop the cascade of events that trigger calcification, fibrosis, and eventually hair loss…
But because calcification and fibrosis are further downstream to DHT, and because calcification and fibrosis are chronic progressive conditions, then reducing DHT won’t actually reverse these conditions! It’ll only slow or stop their progression. This is why Finasteride is great at arresting hair loss, but not at regrowing much hair.
Try Using The Flowchart!
We can use this flowchart to explain the results and shortcomings of almost every hair loss drug on the market.
If you understand a drug’s mechanism (how it works), you can look at the flowchart and evaluate which part of the hair loss cascade it addresses.
Let’s try it with the drug Spironolactone, a “caffeine” topical, and even a full-on hair transplant.
Spironolactone works by blocking our androgen receptors so that DHT can’t accumulate in our scalps. This might help arrest hair loss, but since it doesn’t address pre-existing calcification or fibrosis, it’s limited in completely reversing the condition.
Caffeine topicals help boost blood flow to our follicles. But decreased blood flow is the result of calcification and fibrosis buildup, and unless we reverse those conditions and their triggers, the benefits of boosted blood flow will be short-lived.
Hair transplants work by transplanting healthy hair follicles from the back of your head to thinning regions. But since thinning regions are ridden with calcification and fibrosis, transplanted hairs may eventually thin too – which is why so many people experience failed hair transplants.
Every treatment’s biggest hurdle is calcification and fibrosis. Without reversing these two chronic progressive conditions, any drug, supplement, topical, or therapy targeting hair loss will only be mildly effective.
Calcification And Fibrosis Are The Two Biggest Hurdles To Hair Recovery
If we want to regrow lost hair, we need to restore the environment of the scalp back to its original state – reversing calcification and fibrosis – and restoring blood flow to dormant follicles so they can turn terminal once again. It’s definitely not an easy path forward, but it’s possible.
Beyond Hair: Why Calcification And Fibrosis Matter
If you’re suffering from hair loss and you think that calcification and fibrosis are only happening on top of your scalp, you’re probably wrong.
Calcification and fibrosis can happen in vessels and soft tissues everywhere in our bodies. And in fact, pattern baldness is closely associated with heart disease. As an article from Harvard states:
“Calcium can accumulate in the arterial plaque that develops after an injury to the vessel wall. The plaque is usually soft to begin with, but eventually tends to harden and become calcified.”
If we eliminate the triggers of calcification and fibrosis, we’re not just targeting hair loss… We’re also helping to halt the progression of calcification in other parts of our bodies. We’re positioning ourselves to become healthier, happier, and longer-living.
It’s Easy To Prevent Calcification. It’s Hard To Reverse It.
It’s much easier to prevent calcification and fibrosis than it is to reverse these conditions.
For instance, the right diet can significantly stop the development of calcification, but diet rarely reverses calcification. This is why, in most cases, dietary changes don’t result in significant hair regrowth. So the next time you see an ad claiming “one simple diet trick” can regrow hair, don’t buy into it.
Final Takeaways
Many people try to make hair loss sound like a “one cause, one solution” problem – but this just isn’t reality.
Calcification and fibrosis are the two biggest hurdles to hair recovery.
Drugs like Finasteride decrease scalp DHT, but they do little to reverse any of the calcification and fibrosis already present in our scalps. As a result, most hair loss drugs only slow or arrest hair loss. They don’t necessarily regrow any hair.
Questions? You can reach me in the comments section any time.
Rob English is a researcher, medical editor, and the founder of perfecthairhealth.com. He acts as a peer reviewer for scholarly journals and has published five peer-reviewed papers on androgenic alopecia. He writes regularly about the science behind hair loss (and hair growth). Feel free to browse his long-form articles and publications throughout this site.