In 2007, I asked a dermatologist if low blood flow or poor circulation causes hair loss. He answered with a firm no. He told me that when he cuts into a balding scalp, it bleeds… a lot. He mentioned that the scalp is one of the most densely vascularized regions in the entire body — and as such, there’s just no way a restricted blood supply could cause androgenic alopecia (or pattern hair loss).
At first, I accepted the argument. After all, scalp tissues do have a dense capillary network. Accordingly, scalps have about ten times the blood flow of other anatomical regions. Scalps also bleed excessively during surgery… yet men and women still lose hair there.
So, maybe poor circulation or low blood flow doesn’t cause androgenic alopecia (AGA).
But at the same time, a lot of evidence contradicts with this statement.
For instance, hair requires blood, oxygen, and nutrients to grow. And this study revealed that balding scalps have 40% less oxygen than non-balding scalps. Blood carries oxygen, so presumably, balding scalp tissues also have lower blood flow…
And they do! This study demonstrated that compared to non-balding scalps, balding scalps have 2.6 times less subcutaneous blood flow! And if blood supply is what fuels hair growth, then it make sense that lower blood flow would lead to hair loss.
This concept isn’t new to most readers here. I’ve written about the hair loss-blood flow connection before. I’ve also published a paper touching on the topic. And in these writings, I tend to convey a pretty straightforward argument: that low blood flow does cause pattern hair loss.
But the truth is… I was oversimplifying things. The science is far more nuanced and complex than I suggested. In fact, it’s not entirely clear what role poor circulation has in AGA… if any at all.
This article explains why. And this time, no simplifications. We’re diving into the circulation-AGA connection and all its nuance. And just as a heads up — this article gets a little technical.
First, we’ll uncover a major study that led scientists to conclude that poor circulation doesn’t cause AGA. In other words, we’ll build the strongest opposition to the idea that reduced blood flow causes pattern hair loss. Then we’ll build the counterargument — revealing new findings that contradict a 50+ year-old belief about the blood flow-hair loss connection.
Finally, I’ll explain where I stand on the issue — and why, when it comes to reversing AGA, improving blood flow is incredibly hard. By the end, we should have gained a firm understanding of the hair cycle, how it influences scalp blood flow, where AGA morphology comes into play… and why these factors make it so hard to parcel out causation from correlation for poor circulation and AGA.
If you have any questions, please reach out in the comments!
Does low blood flow cause AGA? Maybe not.
The blood flow-AGA debate isn’t new. It’s as old as Roman times, with Julius Caesar reportedly believing his own male pattern baldness was due to poor scalp circulation. But it wasn’t until 1959 that investigators attempted to evaluate (in a scientific setting) whether this belief held merit.
The experiment was simple: using cadavers, researchers took biopsies of human scalp skin. Then, under a microscope, they examined the scalp skin’s hair follicles (and hair) and attempted to answer a simple question:
As a hair transitions into later stages of the hair cycle, what causes the degradation of that hair’s blood supply?
In reality, that’s not a simple question. But if we’re to understand the relationship between blood flow and pattern hair loss, we need to also understand the hair cycle… and why, when it comes to AGA pathology, answering this “simple” question is so important.
What is the hair cycle?
Our hairs are in a constant state of growing, shedding, or regenerating. This phenomenon is known as the hair cycle. And hair loss researchers like to think about the hair cycle in three stages: anagen (growth), catagen (resting), and telogen (shedding).
To identify the “stage” of any hair, we need to biopsy the scalp skin, look under a microscope, and answer two questions:
- Is the hair still growing?
- Is the hair still connected to its main blood supply?
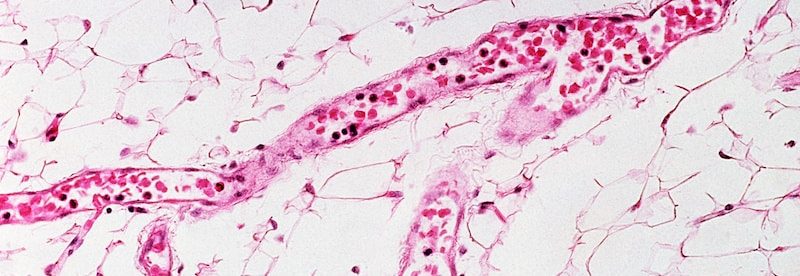
And that means we need to look at our scalp skin from this angle (i.e., a biopsy):
Note in this graphic: those blue and red lines are small microvascular networks. Those networks are the main blood supply of the hair. And that seed-like cluster at the hair base? That’s called the dermal papilla.
The dermal papilla is what connects the hair follicle to its microvascular network. It’s sort of like the hair’s powerhouse. The dermal papilla takes in energy (i.e., blood, nutrient, and oxygen from the microvascular networks) and turns that energy into hair growth. It goes without saying that in the absence of a dermal papilla, hair cannot grow.
Knowing this, we can better define the three stages of the hair cycle. After all, each hair “stage” is defined by 1) whether a hair is still growing, and 2) the connection of that hair to the dermal papilla.
- Anagen (growing) (~85% of our scalp hair). Anagen hairs are growing, and still firmly connected to the dermal papilla.
- Catagen (resting) (~1% of our scalp hair). Catagen hairs are not growing, and their dermal papilla is beginning to descend away from the hair base.
- Telogen (shedding) (~10-15% of our scalp hair). Telogen hairs are not growing and are ready to fall out at any moment. Moreover, their dermal papilla has completely detached from the hair base. With 10-15% of our scalp hair in the telogen stage, this is why we lose 100+ hairs daily (even in the absence of pattern hair loss).
Once a telogen hair sheds, the dermal papilla regenerates and forms a new anagen hair… and the cycle repeats. In fact, here’s a graphic showing all three hair cycle stages:
Again: as the hair moves from anagen to catagen, the dermal papilla shrinks and descends away from the hair base… as does the hair’s blood supply.
This is important. Why? Because as the dermal papilla and blood supply shrink, so does the amount of blood pumping to the hair follicle. That means that hairs in catagen (resting) have less blood supply than hairs in anagen (growth).
Why is this relevant to AGA?
Well, when a hair begins to miniaturize during AGA, they reach a point where they become “stuck” in a catagen- or telogen-like state. For instance, according to this review, we see…
- Reduced hair follicle size and hair length
- Reduced dermal papilla size
- Reduced / degenerating micro-capillary networks to the dermal papilla
Thus, if we want to understand the order of events in AGA (i.e., if blood flow causes pattern hair loss), we need to understand what happens first as a hair enters into categen (resting). Specifically…
Does a hair stop growing after… or before that hair’s microvascular networks degenerate?
If hair growth stops after its blood supply degenerates, this implies reduced blood supply might’ve caused the hair to stop growing. If a hair stops growing before, this suggests reduced blood flow is not the cause of hair loss, but the effect.
This is what that 1959 study attempted to answer. Hence the researchers’ question:
What causes the reduction in blood supply as a hair enters into the catagen stage of the hair cycle?
And now we can begin to uncover the answers.
Do catagen hairs stop growing before or after their blood supply degenerates?
At first, the answer seems obvious. Let’s think about it…
Micro-capillary networks supply nutrients to the dermal papilla — the “powerhouse” of a hair follicle. If the power to that powerhouse (i.e., the blood vessels) decreases, then the output of that powerhouse (i.e., hair growth) must also decrease. So we should presume the order of events is…
- Capillary networks connected to the dermal papilla begin to degenerate, thus reducing nutrient transport, blood, and oxygen supply to the dermal papilla.
- In response, the dermal papilla shrinks to compensate for lower energy intake, and starts to descend from the hair.
- Eventually, the dermal papilla detaches from the hair entirely — disconnecting the hair from its powerhouse — causing the hair to stop growing.
This is a logical, well-reasoned sequence of events. And before researching AGA and hair cycle disorders, I believed it to make sense. There’s just one issue…
It’s 100% wrong. In fact, that 1959 study proved it. Shockingly, these researchers discovered — contrary to what was expected — that a hair actually stops growing before its capillary network (i.e., blood supply) degenerates.
Hair stops growing before its blood vessels degenerate.
That’s right. According to that study, the order is actually…
- A hair stops growing, and resultantly…
- The dermal papilla and capillary networks degenerate and eventually disconnect from the hair base.
This means that scalp blood flow decreases after a hair stops growing. And it bears emphasizing: this is completely unintuitive (at least to me).
Why? Let’s go back to our powerhouse analogy. Saying that a hair stops growing before its capillary networks degenerate is like saying that a box of chocolates stopped making itself so its factory workers (the dermal papilla and blood supply) could skip work the next day. It makes no sense.
And yet this is exactly what happens in our own scalps. In fact, here’s the quote from the paper:
These observations indicate that the degeneration of the blood vessels in the dermal papilla during catagen is a secondary effect and not the primary cause for cessation of hair growth.
What’s more, these findings aren’t just one-offs. They’ve been confirmed again… and again.
Which begs the question…
If a hair stops growing before its dermal papilla and blood supply degenerate, what triggers that hair to stop growing?
Luckily, these investigators identified a few culprits. In the biopsy photos, they noticed three distinct changes in a catagen hair’s surrounding tissue that directly preceded a stop in hair growth. They were:
- Changes to the connective tissue sheath
- Changes to the glassy membrane
- Changes to the external root sheath
Don’t worry about these new terms. All we need to know is where they are. See the below graphic (in the middle-left).
(source)
We can see the connective tissue sheath, external root sheath, and glassy membrane are all next to each other, surrounding the hair shaft. They’re known as mesodermal tissues (i.e., tissues surrounding where the hair grows).
And here’s what these investigators observed:
Right before a hair stops growing, these mesodermal tissues expand and distort. In doing so, they constrict the width of the hair shaft. This constriction pinches the hair, signaling for it to stop growing… which then signals to the dermal papilla and microvascular networks to degenerate.
Again, just to summarize the order. In the catagen phase of the hair cycle…
Mesodermal sheaths expand >> hair shaft gets pinched >> hair stops growing >> dermal papilla and blood vessels degenerate
This means that reduced blood flow comes after a hair stops growing.
And this had huge implications for AGA. Why? Because AGA-affected hairs undergo changes very similar to the ones observed in catagen (resting) and telogen (shedding) hairs. And after all, AGA-affected scalps have lower blood flow than non-balding scalps…
So… what did investigators extrapolate?
Reduced blood flow doesn’t cause AGA… AGA causes reduced blood flow.
This is why, in literature reviews, so many AGA investigators state that reduced blood flow in AGA happens after the hairs start to miniaturize. In other words, low blood flow is the effect of AGA… not the cause.
However, we’ve only built the strongest opposition to the “poor circulation causes hair loss” argument. In other words, we’re still missing the other half of the debate!
And if you haven’t already noticed, there’s one major problem with the opposition’s logic…
Hair cycling and AGA are not synonymous.
Androgenic alopecia (AGA) is characterized by the following three traits:
- Hair follicle miniaturization. In affected regions, the diameter of each hair strand gets progressively thinner.
- Increased telogen:anagen ratio. In affected regions, ratio of shedded versus growing hairs increases.
- Increased anagen cycling. In affected regions, hairs grow for shorter time periods before they cycle into resting.
Yes, the hair cycle is undoubtedly involved in this process. For instance, many researchers argue that the step-process for hair follicle miniaturization is as follows:
- A hair strand disconnects from its hair follicle base (catagen)
- The hair sheds (telogen), and the follicle degenerates (loss of blood flow)
- A new hair follicle is created where the old one once was (new anagen), but…
- That follicle has a smaller dermal papillae cluster, and thereby produces a smaller hair follicle, which produces a tinier hair strand
And again, this is why some researchers believe low blood flow is a consequence (and not a cause) of AGA. If a hair strand disconnects from its hair follicle base before that hair follicle degenerates (and thereby loses blood flow), then this would imply that the loss of blood flow is a consequence of the hair shedding… not the other way around.
This is true, but only if we maintain a myopic view of everything that happens in a balding scalp.
If we actually expand our vantage point to the entire scalp itself, it becomes clear there’s much more to discuss… and many other places where scalp blood flow is reduced.
Which brings us to our counterargument.
The evidence that reduced blood flow causes pattern hair loss
The problem with scalp biopsies
Before moving forward, it’s important to note that nearly everything we know about hair loss “histology” – i.e., what hair loss disorders look like underneath the skin – comes through research on scalp biopsies. In living subjects, these are small “punch” incisions – generally no more than 4mm x 4mm – where someone is losing their hair. Investigators will take these tissue samples, examine them under a microscope, and use the histological presentations of the sample to make a better hair loss diagnosis.
Scalp biopsies are incredibly useful tools, but they require an important caveat: they only provide a 4mm x 4mm perspective of the balding process. These biopsies create somewhat of a myopic bias in the research of hair loss pathophysiology: we’re only looking for the “cause-and-effect” of hair follicle miniaturization in the regions directly surrounding the hair follicle. This begs the question:
What if we expand our view and look at the histology of the entire scalp?
When we do this, we see that there’s another key region in which blood flow is reduced… one that might even contribute to the three defining characteristics of AGA: hair follicle miniaturization, increased telogen:anagen ratios, and increased anagen cycling.
It’s the scalp perimeter muscles.
Some evidence suggests that 80% of men with AGA have involuntarily chronically contracted scalp perimeter muscles
The blood supply for our extremities (i.e., our hands and feet) originate from one place: the heart. Our scalps are no different. And that means that the blood supplying the tops of our scalps (i.e., hair follicles) must originate from below, and must travel up.
Blood vessels develop through paths of “least resistance”. And that means that the blood vessels that support the tops of our scalps originate from below… and must pass through the muscle tissues along the perimeters of our scalps.
While researching botulinum toxin (i.e., Botox) as a treatment to relieve tension headaches, Dr. Freund noticed that his male and female patients with AGA (including himself) also had extremely tight scalp perimeter muscles.
Anatomically, when a muscle is flexed, it expands against its surrounding tissues… much like the mesodermal sheath expands against the hair shaft. And like the mesodermal expansion, chronic muscle contract also has a consequence: the pinching and compression of its blood vessel networks. Specifically, the blood vessels that supply the top parts of our scalps… the region where we suffer from pattern hair loss.
Interestingly, the investigators of this study revealed that balding scalps have 40% less transcutaneous oxygen than non-balding scalps… and postulated that the drop in oxygen levels couldn’t be due to hair cycle changes alone. And more importantly, that same study showed that when oxygen levels drop below a certain threshold, fibrosis forms… the same fibrosis we see in AGA.
Dr. Freund hypothesized that the chronic contraction of the scalp’s perimeter muscles might be the cause of this reduced blood flow. After all, this chronic muscular contraction should theoretically pinch the capillary networks which supply blood to AGA tissues, thereby constricting their flow and decreasing oxygen, blood, and nutrient levels.
So Dr. Freund set out to test his hypothesis. He injected a group of AGA-affected men with Botox – a neuro-modifier that forces muscles to relax. He made these injections into all the muscles lining the perimeter of the scalp. And six months later, when the effects began to wear off, he brought these men back in for another round of injections.
After almost a year, the men came back in to gauge their change in hair count. The results: a 75% response rate for the treatment group… and an 18% increase in hair count in less than a year.
For what it’s worth, Dr. Freund’s research has been validated again and again. And interestingly, the response rates to these studies all seem to land around 80%.
In other words, 80% of men with AGA saw hair loss improvements after taking their scalp perimeter muscles out of chronic contraction, and thereby purportedly unclamping the arterial branches running through these muscles to improve blood flow to the top of the scalp.
And what does that suggest? Two things:
- For ~80% of men with AGA, reductions in blood flow don’t just occur as a consequence of increased hair cycling and hair follicle miniaturization; they also occur because the scalp perimeter muscles might be pinching arterial passageways and thus restricting blood supply to the top of the scalp.
- For ~80% of men with AGA, relaxing these muscles improves hair growth… and at a significant magnitude.
To me, this evidence suggests that we cannot use research on the hair cycle to claim that low blood flow is a consequence of AGA, not a cause. Rather, if we expand our vantage point to the rest of the balding scalp, it’s possible that reduced blood flow might also occur as a result of the clamping of arterial branches… and that by unclamping these branches through muscle relaxants like botulinum toxin, we might improve blood flow and thereby improve AGA outcomes.
Therefore, low blood flow is probably both a cause and consequence of AGA, depending on where you’re looking. It’s a consequence directly surrounding hair follicles, and potentially, also a cause if we zoom out and look at blood flow reductions to the entire scalp from the pinching of arterial branches surrounding the scalp perimeter muscles.
Another potential contributing factor: how muscular contractions may also trigger chronic scalp tension (and chronic inflammation)
To emphasize, this is all hypothetical, and getting into the details here requires a separate article. But here are the highlights:
In 2015, this research team demonstrated that when muscles surrounding our scalp perimeter contract, they form a tension pattern at the top of our scalps that closely aligns with the pattern and progression of AGA. Here’s the model:
As we already know, chronic tension can be interpreted in the body as inflammation. And interestingly, this might have implications in AGA.
Resultantly, inflammatory models suggest that our bodies often try to “respond” to inflammation by sending signaling proteins (i.e. TGF-B1) and hormones (i.e., DHT) to resolve the insult. But if this tensile model holds true, then since inflammation in AGA would then be partly tension-derived — and not injury- or infection-derived — our bodies can’t resolve it with an inflammatory response. The end-result: a chronic, low-grade attempt at resolving inflammation that can only be resolved by relieving tension.
Eventually, this chronic inflammation would result in the accumulation of scar tissue. Specifically, fibrosis in mesodermal tissues. And just like mesodermal sheath expansion in the catagen phase of the hair cycle, any additional accumulation of tissue in these regions will constrict hair shaft space… leading to the progressive miniaturization of hair.
In this model, the order of operations looks like this:
Scalp muscles contract >> tension generates across top of scalp >> inflammatory response >> fibrosis in mesodermal sheath >> mesodermal tissue expansion >> hair shaft constriction alongside reduced blood flow >> hair loss.
This is why I believe that poor circulation might also be a cause of pattern hair loss. And this is why I still stand by the AGA pathology model I proposed in my paper:
Summary
End-stages of the hair cycle (i.e., catagen and telogen) share histological similarities with parts of AGA progression. Resultantly, some investigators use histological studies on the hair cycle to try and explain the order of events in AGA. This has been especially true for determining if reduced blood circulation is a consequence of AGA… or a cause.
As a hair enters the catagen (resting) phase of the hair cycle, the order of operations is as follows: mesodermal tissues surrounding the hair shaft expand, thereby constricting hair shaft growth space. This stops hair growth and signals to the hair’s dermal papilla and microvascular networks to degenerate. So in the catagen phase of the hair cycle, hair growth stops before blood flow reduces… meaning that reduced blood flow is an effect of hair loss… not a cause.
AGA scalps have 2.6 times lower subcutaneous blood flow versus non-balding scalps. And since catagen hairs and early stage AGA hairs look so similar, AGA researchers have used catagen findings as a basis to argue that reduced blood flow is an effect of AGA –not a cause. In other words, these researchers surmise that reduced circulation happens after a hair disappears.
However, there are issues with this line of thinking.
The biggest problem is that in AGA, reductions to blood flow might not only occur in the small blood vessels supporting miniaturizing hair follicles. Rather, they might also occur as a result of the pinching of arterial branches that pass through the scalp perimeter muscles. This occurs due to the involuntary and chronic contraction the scalp perimeter muscles. Therefore, in balding scalps, we have reductions to blood flow in (at least) two places.
In fact, studies on Botox as a therapy for AGA demonstrate that by relaxing these muscles (and thereby improving blood flow through these purportedly pinched arterial branches, and thereby the scalp), AGA outcomes improve… and within the ballpark of what we see with finasteride (although no head-to-head study has been conducted!).
Therefore, reduced blood flow might be a consequence of AGA-related hair follicle miniaturization in certain locations of the scalp, and simultaneously, a cause of hair follicle miniaturization in other sections. It just depends on your vantage point.
This evidence implicates both muscular contractions and chronic scalp tension as potential accelerators of AGA. While the jury is still out on just how contributive these factors are, there’s growing evidence that we should not ignore them.
The bottom-line:
- We can’t apply histological research of the human hair cycle to hair loss disorders like AGA.
- In AGA, reduced blood flow is probably a cause and consequence of pattern hair loss, depending on where you’re looking.
Any questions? You can reach me in the comments any time.
Rob English is a researcher, medical editor, and the founder of perfecthairhealth.com. He acts as a peer reviewer for scholarly journals and has published five peer-reviewed papers on androgenic alopecia. He writes regularly about the science behind hair loss (and hair growth). Feel free to browse his long-form articles and publications throughout this site.