The calcium-hair loss connection
The connection between calcium and hair loss isn’t straightforward. On the one hand, no studies have directly examined the relationship between calcium and hair loss. On the other hand, calcium imbalances are common in chronic conditions linked to hair shedding. So, what’s the verdict on the calcium-hair loss connection?
Can low calcium levels cause hair loss? What about high calcium levels? And if yes, by which mechanisms?
This article uncovers the answers. By the end, you’ll uncover:
- The calcium-hair loss connection: where this mineral does (and doesn’t) influence hair loss
- Calcium loading: why supplementing isn’t always the answer
- The two chronic conditions linked to hair loss and a calcium imbalance… and what to do about them.
If you have any questions, please feel free to reach out in the comments.
What is calcium?
Calcium is one of the most abundant trace minerals in the body. It’s most well-known for its role as a building block of teeth and bone. But, calcium does much more than that. It’s a cellular signaling molecule – driving processes from inflammation to skin cell production and the firing of our neurons (1-3).
Calcium: an essential mineral
Interestingly, calcium also influences our endocrine system: the glands, tissues, and organs that regulate hormone production. And our endocrine systems can influence nearly every aspect of biology, including the development of common hair loss disorders like androgenic alopecia (AGA) and telogen effluvium.
This is why so many people wonder if calcium plays a role in hair loss. The thinking is as follows: calcium levels influence our hormone production, and hormones influence hair loss. So maybe calcium imbalances can cause hair loss.
But is this actually true? Let’s dive into the evidence.
Can a calcium deficiency cause hair loss?
Necessary disclaimer: at the extremes, anything can cause hair loss. For example, a water deficiency can cause hair loss. If we don’t drink water, we die. If we’re dead, we can’t grow hair.
The same is true for most vitamins, minerals, and nutrients – including calcium. If we don’t ingest any calcium, we can’t grow bone. If we can’t grow bone, we die. If we’re dead, we can’t grow hair.
I hope you see where I’m going with this – which is that we’re asking the wrong question. Rather than ask, “Can a calcium deficiency cause hair loss?”, we need to ask is, “Can a calcium deficiency within realistic means cause hair loss?”
And to answer that question, we have to dive into the literature. So, what do the studies say about calcium’s role in hair loss?
There are no studies measuring calcium’s role in human hair loss.
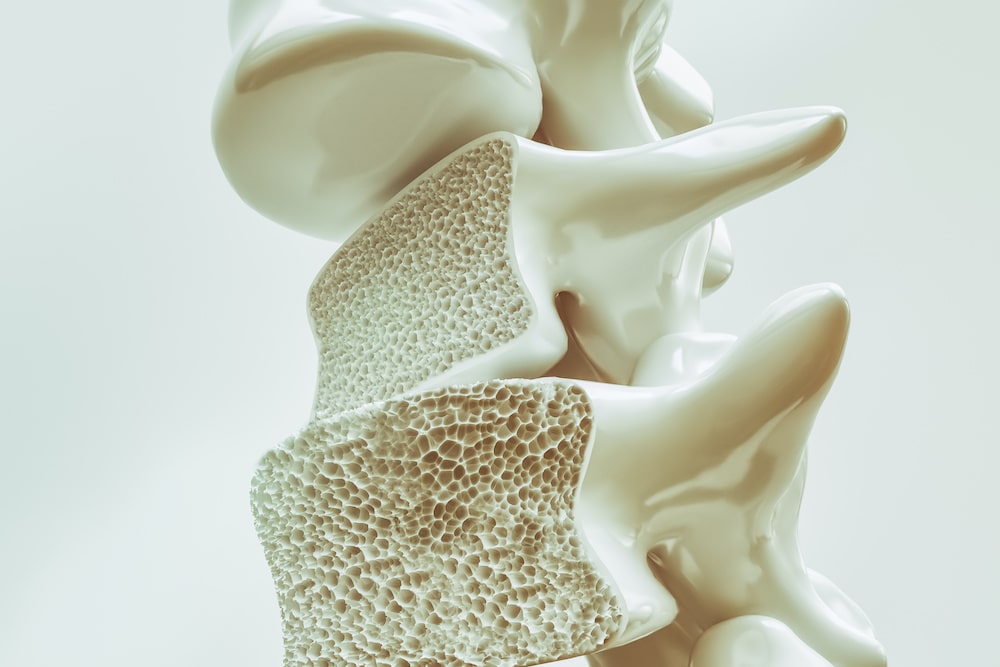
We know that calcium is essential for the function of many tissues. We know that calcium plays a significant role in cellular signaling, a process necessary for maintaining hair growth. And we know that, in animal studies, vitamin D-deficient dogs fed a low-calcium diet develop hair loss (4).
Unfortunately, no studies have directly examined the relationship between calcium and hair loss in humans. That means we don’t yet have data to directly answer this question.
What also makes this complicated: calcium is a tightly regulated mineral. We need calcium to mediate thousands of biochemical processes. In cases of dietary deficiencies, our bodies pull calcium from bone to maintain optimal levels. In cases of dietary surpluses, our bodies expel excess calcium to avoid over-accumulation.
For these reasons, it’s unlikely that – under normal settings – our bodies would let calcium levels to drop low enough to cause problems like bone mineral depletion or hair cycling dysfunction.
But what about abnormal settings?
For example, what about in cases of disease states where our bodies’ nutrient demands are much higher… or nutrient absorption is much lower (i.e., SIBO)… or certain supplements, medications, or surgeries have caused a dysregulation of nutrients in the body?
Under these scenarios, are calcium levels implicated in hair loss? Interestingly, the answer is yes.
Both low and high calcium levels are linked to hair loss – at least indirectly. Here’s how.
The indirect links between calcium imbalances & hair loss
Calcium deficiencies: polycystic ovarian syndrome (PCOS)
Polycystic Ovarian Syndrome (PCOS) is a chronic condition that affects 15-20% of women of reproductive age (5). Its biological biomarkers: high testosterone and insulin insensitivity. Its tell-tale signs: the formation of small cysts on the ovaries, missed or infrequent periods (cycles of 35+ days), weight gain, sluggishness, and even the development of female pattern hair loss – a consequence of the prolonged hormonal imbalances (specifically, the elevated testosterone).
Interestingly, PCOS is also associated with slight (but significant) deficiencies in vitamin B-12, C, D, and calcium (6). This begs the question: are these nutrient deficiencies a cause or a consequence of PCOS?
At least so far, literature reviews suggests that PCOS-related nutrient deficiencies are consequences of PCOS, not causes (7). Specifically, these nutrient deficiencies are partly the result of prolonged insulin resistance, which can increase nutrient demand.
That means that calcium deficiencies do not cause PCOS, and are thereby only indirectly associated with the female pattern hair loss that often accompanies the condition.
Calcium surpluses: hyperparathyroidism
Interestingly, there’s at least one more way that calcium imbalances are indirectly linked to hair loss. In this case, it’s a calcium surplus… and the condition is called hyperparathyroidism.
To explain this, we’ll start by uncovering the parathyroid glands, how this relates to hair shedding, and where calcium comes into play.
The parathyroid-hair loss connection
The parathyroid glands are part of our endocrine system. They consist of four glands that sit right behind the thyroid.
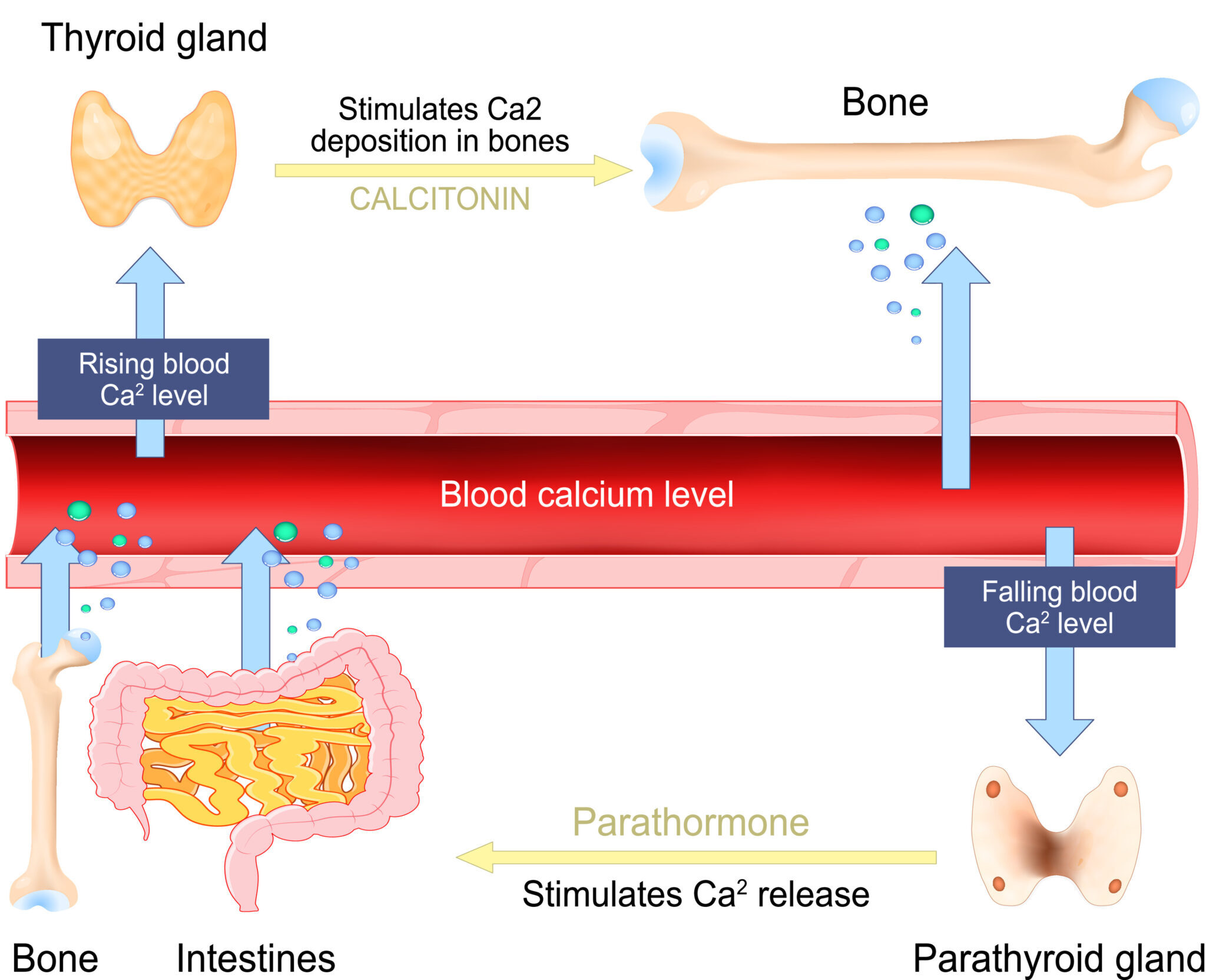
When our blood calcium levels go down, the parathyroid is responsible for getting them back in the normal range. It does this by secreting a hormone called parathyroid hormone (8).
The way this happens is out-of-scope for this article, but in short, parathyroid hormone signals for our bodies to leech calcium from our bone. In leeching bone calcium, blood levels of calcium increase, and the calcium then gets redistributed to other tissues in need.
Parathyroid’s action on bone to maintain calcium homeostasis
However, there are cases where this process can backfire.
Studies have shown that when parathyroid hormone is added to hair follicle cultures, it can cause them to prematurely enter the catagen phase of the hair cycle (9). Catagen is the transition step between the growth and shedding phases of the hair cycle. Therefore, anything that initiates catagen will eventually culminate into hair shedding.
If many hairs enter catagen at once, the hair shedding can be so drastic that it leads to a visible decrease in hair density. This can lead to a temporary form of hair thinning called telogen effluvium.
Hypothetically, this opens up the possibility that chronically elevated parathyroid hormone levels could trigger chronic, persistent hair shedding. Unsurprisingly, hair loss is a common complain amongst those with an overactive parathyroid (9).
So, what causes parathyroid hormone to remain elevated for significant periods of time? And what does any of this have to do with calcium intake?
The parathyroid-calcium connection
When parathyroid hormones go out of range, it is classified as a condition called hyperparathyroidism. There are two types of hyperparathyroidism: primary and secondary.
Primary hyperparathyroidism is almost always caused by a tumor on the parathyroid gland (10). Treatment for this type of hyperparathyroidism is usually confined to removing the affected gland – and through surgery.
Secondary hyperparathyroidism, on the other hand, are characterized as out-of-range parathyroid hormone levels caused by something unrelated to a direct dysfunction of the parathyroid gland itself. As such, its causes are more complex, individualized, and wide-ranging than primary hyperparathyroidism.
One common cause of secondary hyperparathyroidism is chronic kidney disease – which severely impacts the kidney’s ability to handle calcium and vitamin D.
The other common cause of secondary hyperparathyroidism is a vitamin D deficiency (11). Interestingly, vitamin D helps regulate calcium levels in the blood. When vitamin D levels are low, calcium levels in the blood drop. This engages the parathyroid gland to increase secretion of parathyroid hormone, all so that calcium levels can increase.
Low vitamin D >> low serum calcium >> increased parathyroid hormone >> increased calcium leeching from bone >> increased serum calcium
Therefore, hyperparathyroidism is another scenario where we can see imbalanced calcium levels and hair loss. In this case, it’s usually high calcium. But similar to PCOS, the calcium dysregulation is a consequence of the chronic condition, and not a cause of the hair thinning.
If I have secondary hyperparathyroidism, will eating less calcium lower my calcium scores?
Probably not. Here’s a quick overview of the relationship between calcium intake and elevated parathyroid hormones:
- No studies have currently established a link between calcium and secondary hyperparathyroidism.
- One study on almost 60,000 women found that increased calcium intake was independently associated with a decreased risk of developing primary hyperparathyroidism (12). This suggests that, in the long run, consuming adequate calcium may prevent primary hyperparathyroidism caused by tumors.
- Outside of this, some studies (13-15) have suggested that calcium and parathyroid hormones have an inverse relationship. In other words, decreased calcium intake may lead to increased parathyroid hormone levels while increased intake leads to lower parathyroid levels. However, this increase doesn’t lead to parathyroid hormones going out of range.
From this, we can glean three things: (1) adequate calcium intake may prevent primary hyperparathyroidism, but (2) poor calcium intake doesn’t appear to cause secondary hyperparathyroidism, and (3) decreased calcium intake may lead to increased parathyroid hormone (however, this doesn’t likely lead to hyperparathyroidism).
So, when we look at the big picture, it seems that poor calcium intake isn’t strongly associated with hyperparathyroidism as both a cause or a treatment. Rather, it elevates parathyroid levels, but not too far outside of the normal range.
Therefore, if you’re dealing with hair loss and you have high (or low) calcium scores, consider getting tested for vitamin D, PCOS, and hyperparathyroidism. In the interim, make sure to eat adequate amounts of calcium.
The good news is that for most modern diets, getting enough calcium shouldn’t be too hard.
How to optimize calcium intake
In general, I’ve always felt best to get nutrients from foods as opposed to supplements. In the case of calcium, this is especially important. Here’s why.
Calcium supplementation has been linked to an increased risk of cardiovascular events (16). In some cases, calcium supplements can also disrupt the pH of the stomach, which is critical for optimal digestion and nutrient assimilation (and, thus, hair growth) (17).
The good news is that calcium is readily available in the diet – even if you’re not currently consuming dairy. Here are just a few non-dairy foods replete with calcium:
| Food sources of calcium (RDI: 1,000mg) | |
| Food source, serving size | Mg, % DV |
| Egg shells (3g) | 1,200mg, 120% |
| Firm tofu (100g) | 683mg, 53% |
| Black eyed peas (100g) | 128mg, 10% |
| Okra (100g) | 77mg, 6% |
| Trout (100g) | 86mg, 7% |
| Acorn squash (100g) | 44mg, 3% |
For most adults consuming a balanced diet, you’re probably getting enough calcium. However, if you want to be sure about your calcium intake (and other nutrients), you can always track the micronutrient sufficiency of your diet using Cronometer or FitDay.
Summary
Calcium is an essential nutrient. But aside from extreme deficiencies, calcium imbalances don’t appear to cause hair loss.
There are no human studies examining the role of calcium levels and hair loss. However, calcium is indirectly related to hair follicle cycling. Moreover, studies have shown that vitamin D-deficient animals fed a low calcium diet develop alopecia. Therefore, it’s not unreasonable to wonder if calcium plays a role in hair loss.
To date, there are only two scenarios where calcium imbalances are linked to thinning hair:
- Low calcium and hair loss observed in polycystic ovarian syndrome patients
- High calcium and hair loss observed in hyperparathyroid patients
But in both situations, the calcium imbalances are consequences of the condition, rather than the cause of the hair loss.
Evidence shows that dietary calcium has little-to-no impact on blood calcium levels, at least within normal boundaries. Having said that, calcium supplementation may lead to an increased risk of heart disease – and potentially as a direct consequence to increased arterial calcification. For these reasons, it’s generally best to avoid calcium supplements altogether and stick to food sources (if possible).
The bottom line: calcium likely plays little to no role in the overwhelming majority of hair loss cases. If you’re dealing with hair loss and you have high (or low) calcium scores, consider getting tested for vitamin D, PCOS, and hyperparathyroidism. You might save yourself a lot of time, energy, and hair.
Questions? Comments? Please reach out in the comments section below.

Rob English is a researcher, medical editor, and the founder of perfecthairhealth.com. He acts as a peer reviewer for scholarly journals and has published five peer-reviewed papers on androgenic alopecia. He writes regularly about the science behind hair loss (and hair growth). Feel free to browse his long-form articles and publications throughout this site.


Thank you very much for the free course. I look forward to receiving it.