Helminths are parasitic worms that live in our intestines. Once maligned by the medical field (and eradicated in most of the developed world), studies now suggest that helminthic worms may have “co-evolved” with humans. They might even help regulate our gut flora, immune systems, and hormones.
Today, researchers are wondering if the absence of helminths inside our “modern” guts might explain the rise in conditions like ulcerative colitis, multiple sclerosis, and maybe even certain hair loss disorders.
In this article, we’ll dive into the science surrounding helminthic worms, their relationship to autoimmunity, and their potential role in hair loss and hair growth. We’ll also reveal findings from clinical trials on helminthic therapy: deliberate inoculation with helminthic worms – specifically, hookworms – to treat food allergies and autoimmune conditions.
Finally, we’ll uncover anecdotes of helminths and hair growth, outline the future of helminthic research, and reveal if hookworms may one day be used to treat hair loss disorders like alopecia areata and androgenic alopecia.
If you have any questions, feel free to reach out in the comments.
Aren’t all parasites dangerous?
When we think of parasites, we often think of illness: a tapeworm infection from eating raw sushi… a case of schistosomiasis from swimming in a tropical lake… a bout of trichinosis from ingesting undercooked pork.
In reality, the relationship between parasites and human health is much more multidimensional. While some parasites harbor a risk of distress, disease, and death… others may protect us from ailments. For instance:
- Parasites can decrease the severity of illnesses. Some research shows that the parasite, Gardia, can modulate the effects of rotavirus such that it becomes less infective in children [1]. Other studies show that kids infected with moderate amounts of hookworms have less severe malaria infections [2, 3, 4].
- Parasites can help fight off more dangerous parasites. Some parasites – like H. baujardi – may lower the risk of F. hepatica transmission by ~70% (a type of parasitic fluke that causes liver problems) [5].
- Parasites can improve autoimmune symptoms. Some parasites may help calm overreactive immune systems, and in doing so, improve conditions like asthma, irritable bowel syndrome, and perhaps alopecia areata (hair loss). More on this soon.
One parasite that might be both harmful and helpful to humans? Helminths. These worms may play a substantial role in the way that our immune systems behave, and subsequently, our risk to certain diseases and even hair loss.
What are helminths?
Helminths are parasites that live inside the intestines of mammals – including humans.
There are hundreds of helminth species: round worms, flat worms, flukes, and tapeworms. But nearly all of them share two common characteristics:
- They feed off of nutrients from their host (from their blood and food supply).
- They reproduce by “laying eggs” inside the intestinal tract.
Most helminth eggs are then excreted into soil and/or water – where an unsuspected passerby will later come into skin contact with them. The larvae then burrow into the skin, navigate to the new intestinal tract, feed, grow, produce eggs themselves… and the process repeats all over again.
Yes, this may sound gruesome. But, helminth infections are incredibly common. Just look at these estimations for the number of people living with soil-transmitted helminths [6]:
“The four most common soil-transmitted helminths are roundworm (Ascaris lumbricoides), whipworm (Trichuris trichiura), and the anthropophilic hookworms (Necator americanus and Ancylostoma duodenale). Recent estimates suggest that A. lumbricoides infects 1.221 billion people, T. trichiura 795 million, and hookworms 740 million [people].”
In other words, 2+ billion people are infected with helminths. And interestingly, most of these infections are asymptomatic (i.e., the host doesn’t even know they have them).
One of the more common asymptomatic helminthic infections? The anthropophilic hookworm.
These human hookworms reside in the small intestine and grow to ~10 millimeters in length. They’re most commonly found in the developing world where shoe-wearing and sanitization is less stringent – thus allowing for transmission of the hookworm from soil to human.
Fascinatingly, human hookworms may confer a myriad of health benefits – from allergy relief to autoimmune reversal. There are even anecdotes of hookworms improving hair loss. It all has to do with the way in which hookworms survive, and how they can modulate – or dampen – our immune responses.
Human hookworms: how do they influence our immune system?
Human hookworms possess a unique survival capability. Normally, when a parasite enters our body, our immune system fights back by treating the parasite like an infection – inflaming the affected region, inducing a fever, and attacking the parasite – all in hopes of killing it. But when a hookworm enters our body, something different happens.
Instead, hookworms modulate our T-cells [7] (immune cells), tricking our bodies into thinking these parasites are non-threatening [8], so that our immune system doesn’t attack them. In fact, hookworms stay alive in our small intestines by continuously doing this – muting the sensitivity of our own T-cells so that we no longer react to small stressors (namely, the hookworms themselves).
Interestingly, this effect seems to have broader benefits – particularly in relation to our reaction to other mild immune stimulants. One example: allergies.
Human hookworms & allergies
Our bodies encounter small stressors every day, and many of these stressors are at or below the inflammatory threshold of hookworms. To name a few: gluten, peanuts, shellfish, pollen, dairy, and any other common first-world allergy.
When a hookworm modulates our own T-cells to ensure its survival, it also modulates our reaction to these environmental stressors. Preliminary studies now show that in the presence of human hookworms, we often react to these stressors with less inflammation [9]. Therefore, the allergens become less problematic.
On that note, some researchers speculate that allergens are less common in the third world because of helminths and their potentially calming effect on immune reactivity.
How do hookworms modulate our T-cells to reduce allergens?
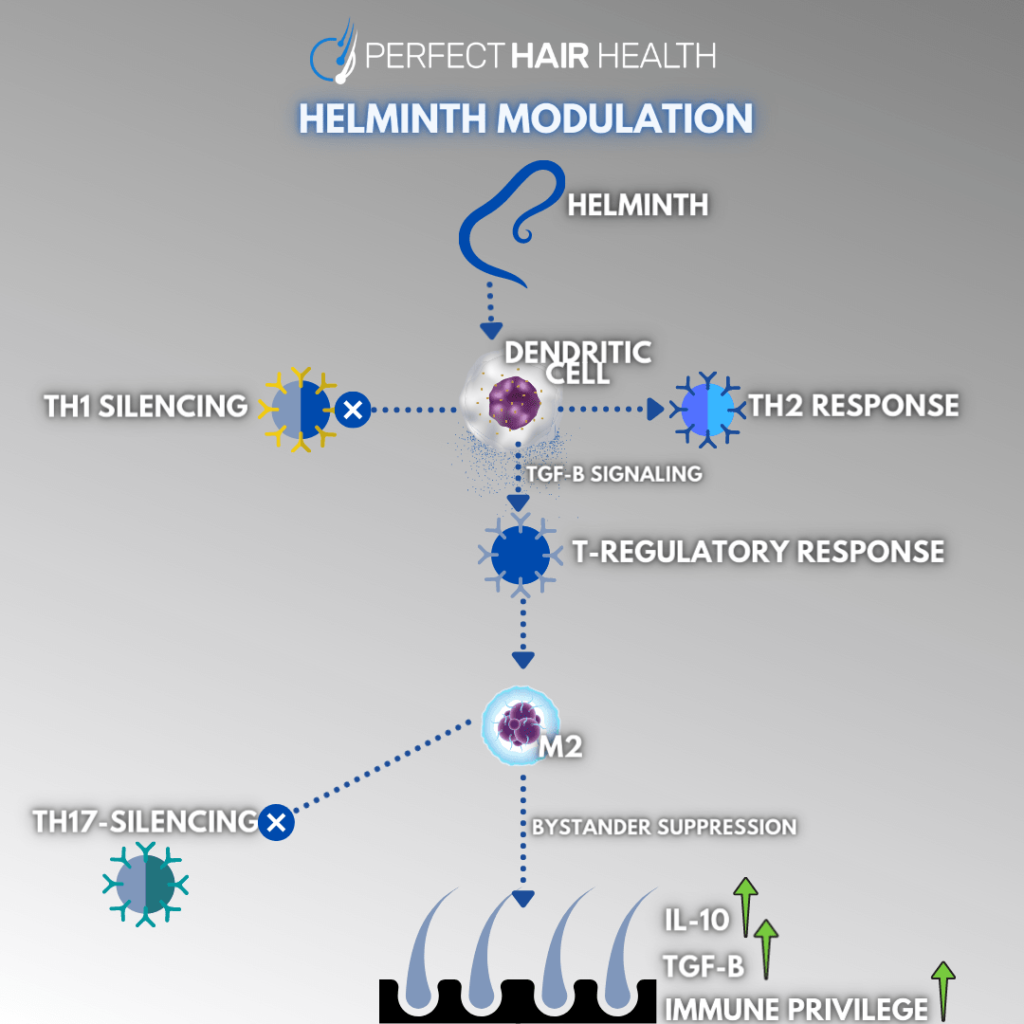
While the exact details are out-of-scope for this article, the gist is that human helminths influence dendritic cell activity. These cells act as messengers between our innate versus adaptive immune systems – i.e., immunity that we are born with versus immunity that we acquire through infections.
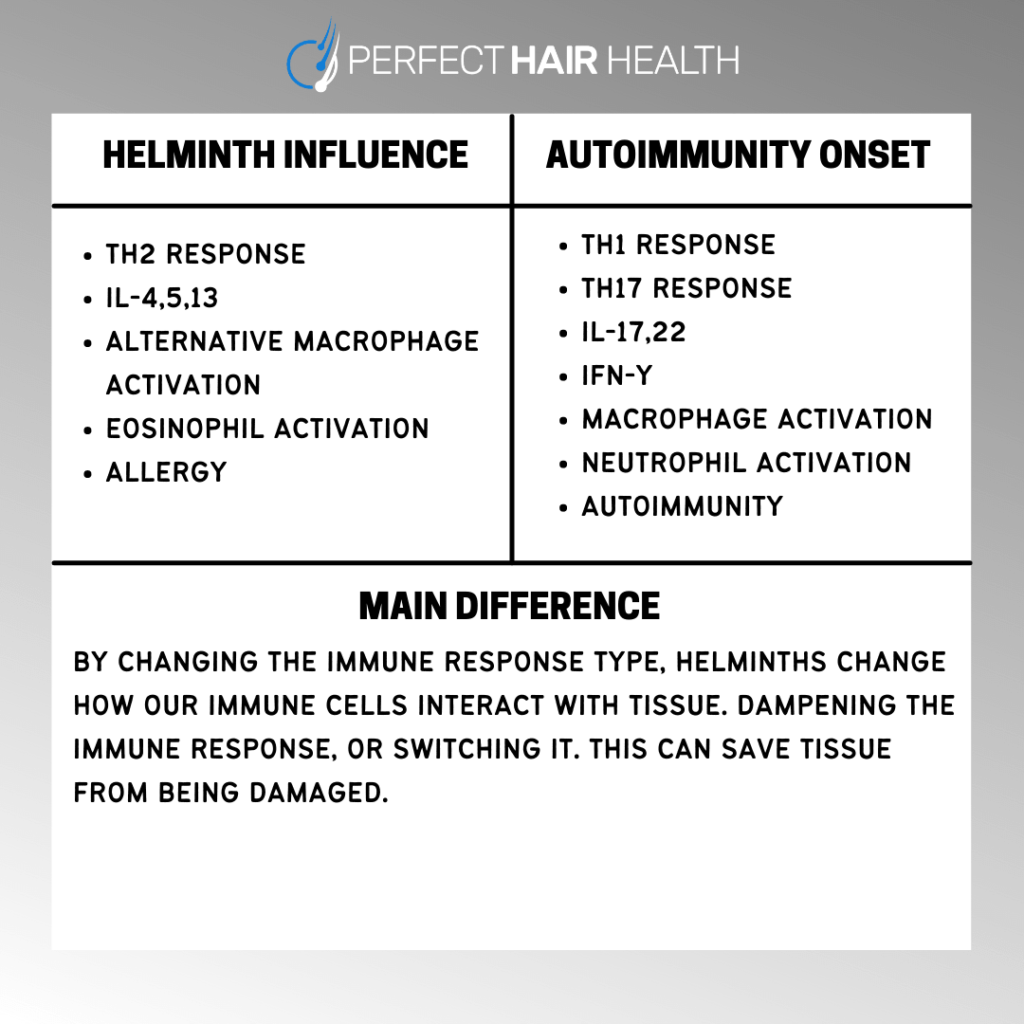
In order to evade detection as a foreign invader, helminths modulate our Th1, Th2, and T-Reg immune responses so that our bodies react less aggressively to foreign stressors – like the hookworm itself.
This has a broader dampening effect on our immune responses – which is why helminthic therapy may not only help to reduce allergens, but also autoimmune conditions themselves.
Human hookworms: a treatment for autoimmunity?
It is estimated that 20-40% of the world’s population has a helminth infection. But in the U.S., that number is closer to 0%. In the last 80 years, sanitation efforts have greatly improved our “parasitic load” – especially compared to hunter-gatherers, early Native Americans, and much of the developing world (where hookworms are often ubiquitous).
At the same time, the incidence of autoimmunity in the U.S. is skyrocketing – and at a pace that far surpasses new diagnostic capabilities or genetics. This begs the question: what have we introduced – or removed – that might explain our explosion in disease?
One possibility: human hookworms. Over the last decade, a growing body of evidence now suggests that humans co-evolved with helminths [10], and that we might be more protected from autoimmune conditions with an infection than without one.
Looking at all of the ways that human hookworms have been shown to modulate our immune system, it’s no surprise why this hypothesis is gaining traction.
In short, we can see the ways in which hookworms influence our immune system have significant overlap with the ways in which autoimmunity develops. Whereas autoimmunity often presents as overreactive Th1 and Th2 responses, hookworms dampen Th1 and Th2 responses. Whereas Th17 is often elevated in autoimmune reactions, hookworms help to reduce Th17 reactivity.
Eventually, researchers decided to stop speculating and start testing to see if deliberate human hookworm infection could improve autoimmune conditions like multiple sclerosis. This is an intervention known as Helminthic Therapy. And so far, the findings have been fascinating.
Helminthic Therapy: autoimmunity study results
Here are just a few studies showing benefit from Helminthic Therapy in the treatment against an array of autoimmune disorders.
- Multiple Sclerosis. Studies on both natural helminth infection and helminth therapy in multiple sclerosis (MS) patients demonstrate that helminths likely have significant beneficial effects in MS, as evidenced by improvements in immunological and brain imaging outcomes [11].
- Crohn’s Disease. Over the course of 24 weeks, 79% of Crohn’s patients administered helminths saw a decrease in the severity of disease [12]. 91% of those patients achieved remission.
- Ulcerative Colitis. Similarly, helminth therapy shows promise in another inflammatory bowel disease: ulcerative colitis — through its ability to modulate intestinal immunological profiles.
What about helminths and hair loss?
Some hair loss disorders are autoimmune in nature. One of the most common autoimmune-driven hair loss disorders? Alopecia areata – which often presents as patchy, rapid-onset hair loss across the scalp.
Example: alopecia areata
Over the past ten years, people with alopecia areata, alopecia universalis, and alopecia totalis have undergone helminthic therapy in an attempt to treat things like allergies and autoimmune conditions. In addition to seeing improvements to these conditions, many have also inadvertently seen improvements to hair growth.
Here are a few anecdotes.
Hookworm / helminthic therapy: evidence for hair regrowth
I first read about a possible connection to helminthic worms and hair loss in an interview with Moises Velasquez-Manoff, who wrote a book entitled, An Epidemic of Absence [13]. In the book, the author details the hypotheses behind helminthic therapy and even his own experience self-infecting with helminths. He’s a sufferer of alopecia universalis — a more advanced form of the autoimmune disorder alopecia areata. When he tried hookworm therapy, he noted the growth of hair for the first time in decades.
Since then, hundreds of others have attempted helminthic therapy – both under doctor supervision and independently through the resources from Helminthic Therapy Wiki page. Occasionally, a side effect reported was the regeneration of hair follicles lost from autoimmune alopecia.
We’ve summarized a few of these anecdotes below. Please keep in mind: anecdotes are synonymous with individual experiences and are generally regarded as low quality in the hierarchy of evidence. Nonetheless, anecdotes often form the building blocks of larger clinical investigations, and are thus worth noting.
Hookworms & hair regrowth: anecdotes from users
“Without a doubt, my treatment with hookworms has been very effective on my bald spots and thinning areas.”
“I have alopecia areata. I have tried helminthic therapy numerous times starting in 2013. My first time around with [hookworms], I took far too many (35) and actually lost loads of hair. Around 2014 I tried HDC in addition to [hookworms] and had great results initially. That lasted for about 5 months then went bad. Hair fell out and I had an increase in joint pain and heart palpitations too. In 2015 I completely stopped [hookworms] and went with plaquenil alone. I struggled with patches coming and going along with other ai issues. This past summer I tried NA again. Things had gotten so bad with my health I didn’t feel I had a lot of options. This time around I did things completely different. I started with 5 NA, I took antihistamines when needed and stayed on my plaquenil. All of my hair loss stopped. It is slowly growing back, a little here and there. The only thing I noticed hair wise is that my eyebrows will thin in spots and coincides with joint pain. Overall though I’m doing so much better. But I am still in 200mg of plaquenil per day.”
-
- Note: Plaquenil is an anti-parasitic drug. In this case, the load of the helminths created an imbalance that did not serve hair regrowth. It’s also possible that the medication itself had beneficial effects in the context of hair loss.
“I have alopecia and have tried helminths on and off for years, both hookworm and hdc. Hookworm actually made it worse and tons of hair fell out. Had good results initially with hdc. I thought they were a miracle at first, but the good effects wore off about 5 months in, when they stopped working and the hair fell out again. I tried the hdc for quite a while, trying to regain the initial results, but I never got the same hair growth again. If I were to try it again for alopecia I would use hdc. I had the best initial response to alopecia with them.”
-
- Note: Hookworm is a parasite that depletes iron from the body. Iron deficiency has been associated with various forms of hair loss as well as thyroid dysfunction, another condition closely associated with forms of hair loss [14,15]. Meanwhile, iron overload, even if not present as the condition hemochromatosis, may exacerbate hair loss symptoms [16]. As such, there appears to be a line denoting the potential ability for hookworm therapy to be effective. In the context of iron deficiency-induced hair loss, further reductions in iron, secondary to helminth therapy, could worsen hair loss. Conversely, in the context of iron overload hair loss, helminth therapy may appear a potential avenue for therapy.
“After starting HDC I regained 80% of all hair within about 4 months.”
“I lost all my hair last year from areata. it started to grow back before taking HDC… but once I started, it bloomed and now I have a full head of hair. I take 30 HDC every two weeks.”
In short, when it comes to the connection between helminths and hair regrowth, evidence is still preliminary, and still growing. But there are at least enough anecdotes to suggest further investigation – especially for autoimmune forms of hair loss.
How might helminths regrow hair?
We can only speculate, but there are a few ways in which helminthic therapy might improve hair loss outcomes for alopecia areata.
- ES-62 secretion
- Restoration of “immune privilege” of hair follicles
- Gut microflora changes
We’ll take these one-by-one.
ES-62 secretion
ES-62 is a protein secreted by parasitic worms (like helminths). This protein seems to exert broad anti-inflammatory effects that influence our immune systems.
In animal models, research suggests that ES-62 secretion modulates microscopic immune signaling proteins, called cytokines. Depending on the cytokine in question, they can be inflammatory or anti-inflammatory.
In ES-62’s case, it’s modulation of cytokines leads to an increase in anti-inflammatory cytokines (IL-10) and a decrease in inflammatory cytokines (IFN-y) [17]. As a result, ES-62 secretion through parasitic worms has shown to be protective against autoimmune disorders like rheumatoid arthritis.
Interestingly, in alopecia areata, IFN-y is also elevated and may even play a role in the development of this hair loss disorder [18,19]. In specific, IFN-y is believed to attract immune cells to the hair follicles, helping to drive an autoimmune attack on hair follicles.
The result? In affected areas, hair follicles rapidly progress from their growth phase to their shedding phase — and many hairs are shed at one time. This leads to what we see on the surface of alopecia areata scalps: patchy, slick-bald spots.
Because helminthic therapy might help dampen IFN-y activity across the body (including hair follicle sites) and IFN-y is believed to contribute to the rapid hair shedding in alopecia areata, it’s possible that helminthic therapy may help to normalize the hair cycle.
As such, it’s theoretically possible that helminthic therapy may help improve the appearance of alopecia areata and even prevent it from recurring.
Immune privilege
Immune privilege is a concept whereby certain tissues require protection against the immune system, as even the slightest bit of inflammation might inhibit that tissue’s regenerative capacity [18,20].
Hair follicles fall under this category. They are believed to have complete immune privilege due to the never-ending hair cycle: the normal degeneration and regeneration of our hair follicles.
In alopecia areata, collapse of immune privilege is a significant contributor to visible hair loss [18]. Some researchers also believe this could be the case for stress-related hair shedding (i.e., telogen effluvium) [21, 22]. As a result, this loss of immune privilege may no longer award the necessary protection from inflammation that is needed for hair follicle regeneration (read: hair growth).
Interestingly, a subset of T-cells called Th17 cells, when elevated, may contribute to this loss of immune privilege [23]. Thus, it comes as no surprise that Th17 cells are elevated in the skin of autoimmune disorders like vitiligo and alopecia areata [24]. Th17 cells are the very same T-cells that helminths help to silence, thereby helping to shut down a pathway that may lead to loss of immune privilege.
Similarly, helminths are known to increase the activity of Treg cells, another subset of T-cells [25]. Unlike Th17 cells, increased levels of Treg activity help in sustaining immune privilege. Thus, helminths may further defend against immune privilege collapse in hair follicles and, therefore, hair loss in alopecia areata and some forms of telogen effluvium.
Gut microflora
Helminths not only help to regulate our immune systems; but they can also influence our gut microbiome: the billions of bacteria that live inside our intestines and influence anything from our hormonal profiles to our food sensitivities.
One way that helminths do this? By encouraging gut microbiome diversity.
Helminths have shown the ability to diversify the gut microbiome. They also seem to affect the activity levels of certain bacterial and viral species [1, 26, 27, 28, 29]. Studies show that gut microflora diversity decreases with age, and that a less diverse gut microbiome seems associated with autoimmune and inflammatory conditions like ulcerative colitis and irritable bowel syndrome [30].
Not surprisingly, studies show that gut microflora imbalances are present in 20-40% of subjects with alopecia areata [31, 32]. If these imbalances contribute to the development of alopecia areata – and if helminths help restore gut diversity – then this may be one under-appreciated way in which hookworms may work to regrow hair lost from alopecia areata.
Helminths, gut bacteria, and DHT: a link to androgenic alopecia?
Our microbiome doesn’t just influence our immune system; it also produces hormones. Specifically, dihydrotestosterone (DHT) – the hormone linked to pattern hair loss (androgenic alopecia). In fact, one study demonstrated that our gut bacteria make at least 70-fold more DHT that the amount of DHT found in our blood – and that this DHT is found inside our intestines and stool samples [33].
It’s unclear if this bacteria-produced DHT can enter the bloodstream and/or influence tissue behavior outside of the intestines. However, it’s hypothetically possible. On that note, hair loss researchers have recently speculated that changes to DHT production inside our intestines might be one reason why some people experience persistent side effects after quitting DHT-lowering drugs like finasteride [34].
On a personal note, I’ve worked with a few individuals with androgenic alopecia who’ve undergone helminthic therapy and later reported a stop in their hair loss. Is this a result of helminths increasing gut microflora diversity, lowering the number of DHT-producing bacteria in the gut, and potentially lowering DHT-related effects elsewhere in the body? With such little research, it’s impossible to say. But it does get us thinking!
On a related note, carnivore diets have also been shown to improve gut flora diversity in n=1 studies. There are case reports of people who arrested male pattern hair loss after adopting an all-meat diet dating all the way back to the 1930’s. Personally, I’ve worked with an individual who saw zero success with finasteride, but who later tried the carnivore diet alongside massaging and experienced great hair regrowth. Here are his photos.
Hair regrowth from a carnivore diet + massaging

So, it’s not outside the realm of possibilities to suggest that helminths might have a similar effect on gut diversity, and thereby improve pattern hair loss outcomes. Without more research, we can only speculate.
Helminthic Therapy: how can we try it?
While you might feel tempted to inoculate yourself with helminths, it is important to note a handful of things:
- Helminthic therapy is based on a handful of studied helminths, with the best-studied species being the hookworm Necator americanus. It’s not a free-for-all inoculation of whichever species you can get your hands on.
- Helminths aren’t always our friends. Sometimes they’re dangerous. Throughout the last century, most studies on helminths have focused on the relationship between parasite and disease [35]. Some helminthic species can trigger neurological diseases like eosinophilic meningoencephalitis (i.e., brain inflammation) [36]. Others can cause severe malnutrition [37]. And some helminths – like pork tapeworm– eat brain tissue and can prove deadly if acquired through undercooked meat [38]. So, if you’re interested in trying helminthic therapy, it goes without saying: it should always be overseen by a medical practitioner.
- We are in no way recommending this treatment. The purpose of this article is to bring light to a potentially novel therapy in the sphere of hair loss, not encourage you to try something that we find fascinating from a hypothetical perspective.
- Purchasing Helminths for the therapy can be difficult to achieve in terms of purity, proper dosing, and selection of the helminths best suited to your needs.
As such the best way to inform yourself and learn how to acquire these organisms is through these resources:
There, you can learn more about the species studied, whether you’re a good candidate for treatment, how you can get your hands on these helminths, and what to expect.
Summary: helminthic therapy for hair loss
Evidence shows that helminths may improve our health in the following ways [39]:
- Immune system. Regulation of Th1/Th2 balance, interleukins, and macrophages.
- Gut microflora. Coexistence with other Eukaryotes, promotion of gut diversity.
- Observed benefits. Reduction of chronic inflammatory states, antibiotic-like activity, anti-allergenic effects potentiated by certain species, improvements to autoimmunity.
In light of this evidence, helminths may also play a role in hair loss (and hair growth).
Some people trying helminthic therapy have reported hair regrowth from conditions ranging from autoimmune forms of hair loss – like alopecia areata. I’ve also worked with people who’ve tried hookworms and reported improvements to androgenic alopecia (i.e., male pattern baldness). While there’s virtually no research into hookworms as a hair loss therapy, it’s theoretically possible that the right parasites might improve a variety of hair loss disorders.
In conclusion, helminthic therapy holds promise within the context of many autoimmune conditions – including hair loss disorders. On that note, helminthic therapy is not something that should be overlooked without serious inquiry. Just as we have utilized probiotics in the modern day for better gut health, there exists the possibility of utilizing helminths in the future for the management of disease – hair loss-related or otherwise.
You can reach us in the comments any time.

Rob English is a researcher, medical editor, and the founder of perfecthairhealth.com. He acts as a peer reviewer for scholarly journals and has published five peer-reviewed papers on androgenic alopecia. He writes regularly about the science behind hair loss (and hair growth). Feel free to browse his long-form articles and publications throughout this site.




Excellent research as always Rob! Wanted to ask if you take a probiotic yogurt supplement? My initial goal was to improve my gut microflora & microbiome as you write about in the book. Wondering if doing so would also accumulate helminth population? I’m about to start on a brand with over 300 friendly nonpathogenic microbial strains / cultures called BRAVO. Learned about it from David Sinclair, a popular anti-aging biologist who teaches at Harvard… and the dude looks like 30 years younger than he is!
Matt, David Sinclair looks his age as a whole or a little bit younger. He does not have a double chin, wrinkles or drooping jowls but that can be achieved by aesthetic surgery.
Hey Matt,
Thanks for reading! Taking a probiotic won’t lead to helminth accumulation – at least if helminths aren’t included in that specific supplement. However, certain probiotics may stave off or encourage the successful inoculation of helminths that enter the gut through foods, egg-to-skin contact, etc. This is because there are species-to-species interactions across helminths and gut microorganisms: some bacteria may make the host environment more favorable, while others may make it more difficult for the helminths to survive.
Best,
Rob
Where can we buy that BRAVO cultures?